Knee Synovitis | Cases
Published on Jan 19, 2021
87 female , 6 month history of knee pain
Difficult weight bearing. Uses 1 walking crutch. Limited flexion and extension ROM due to pain. Swelling present in the whole leg rather than just the knee.
Attended A&E twice due to severity of pain. Was given a knee x-ray.


X-ray Report
Mild degenerative changes noted particularly in relation to the lateral compartment and the patellofemoral joint. A suprapatellar effusion is noted.
No acute bony injury seen.
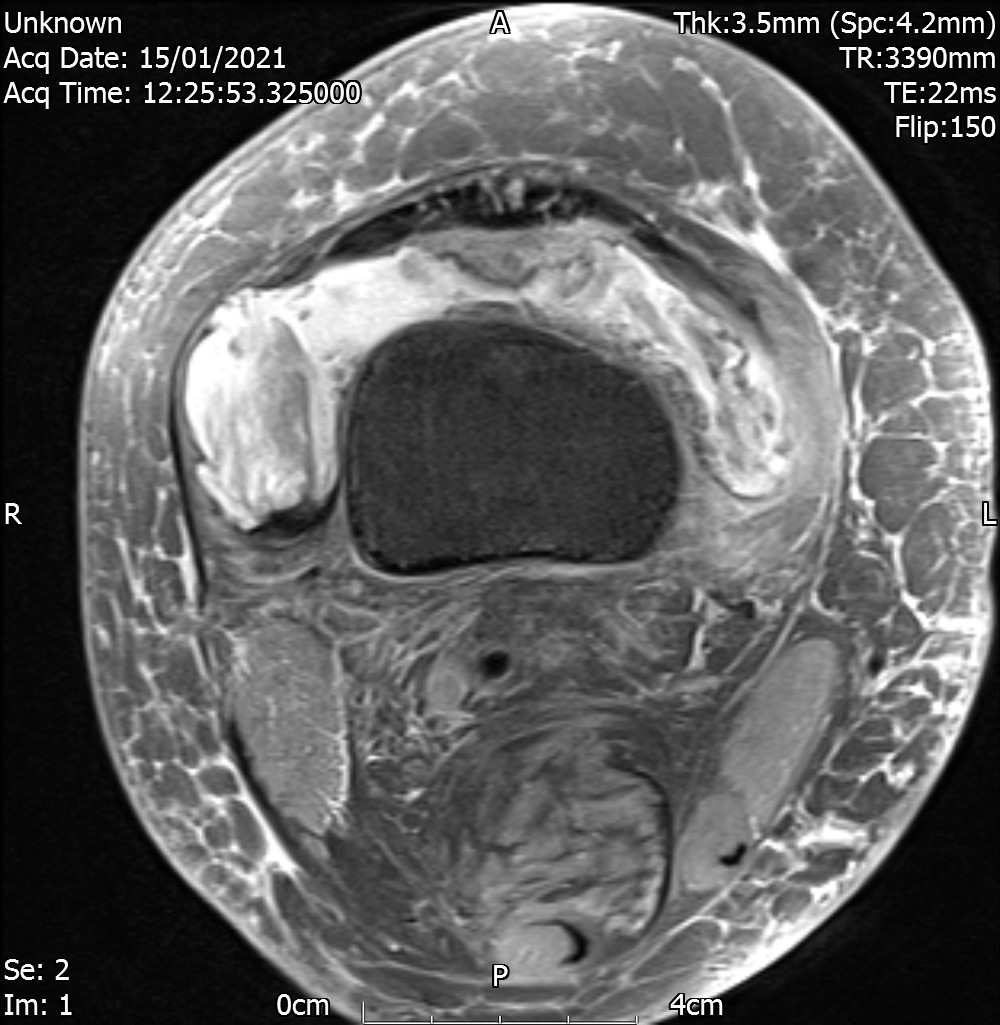
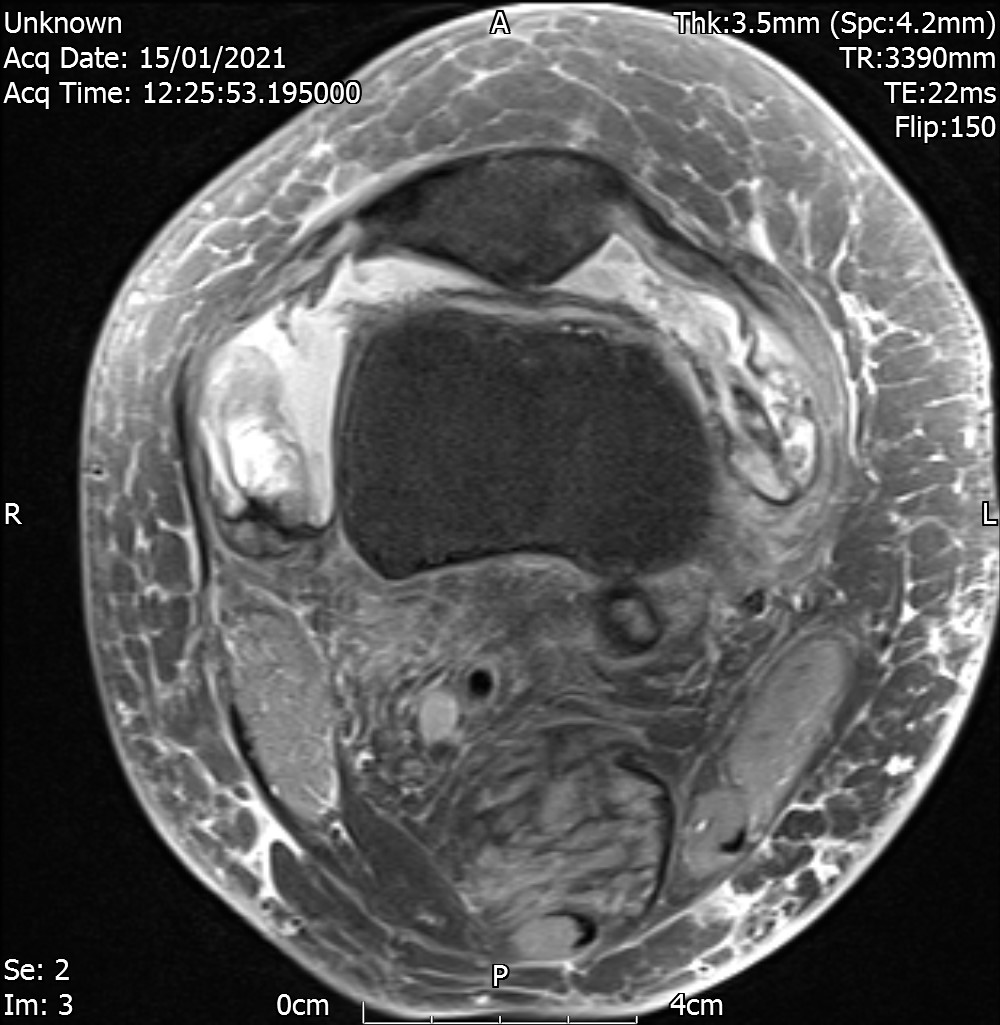
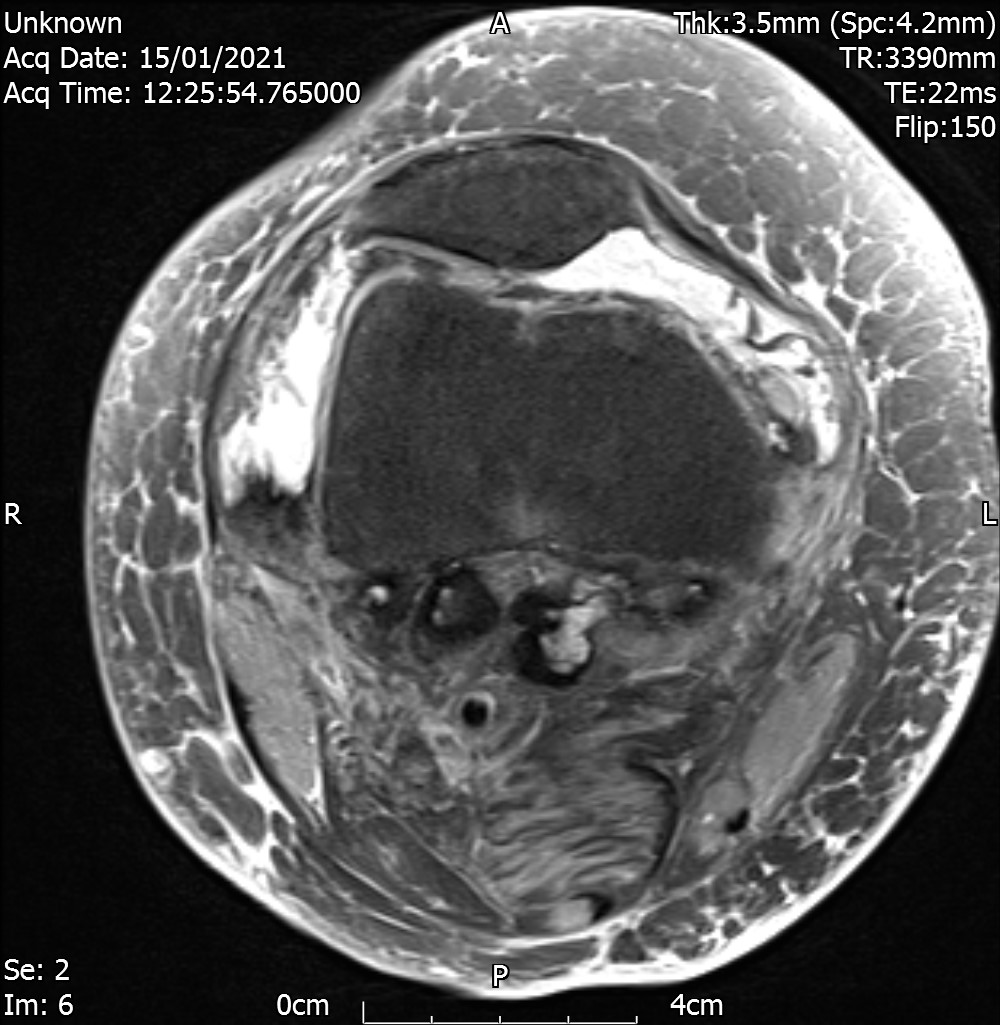
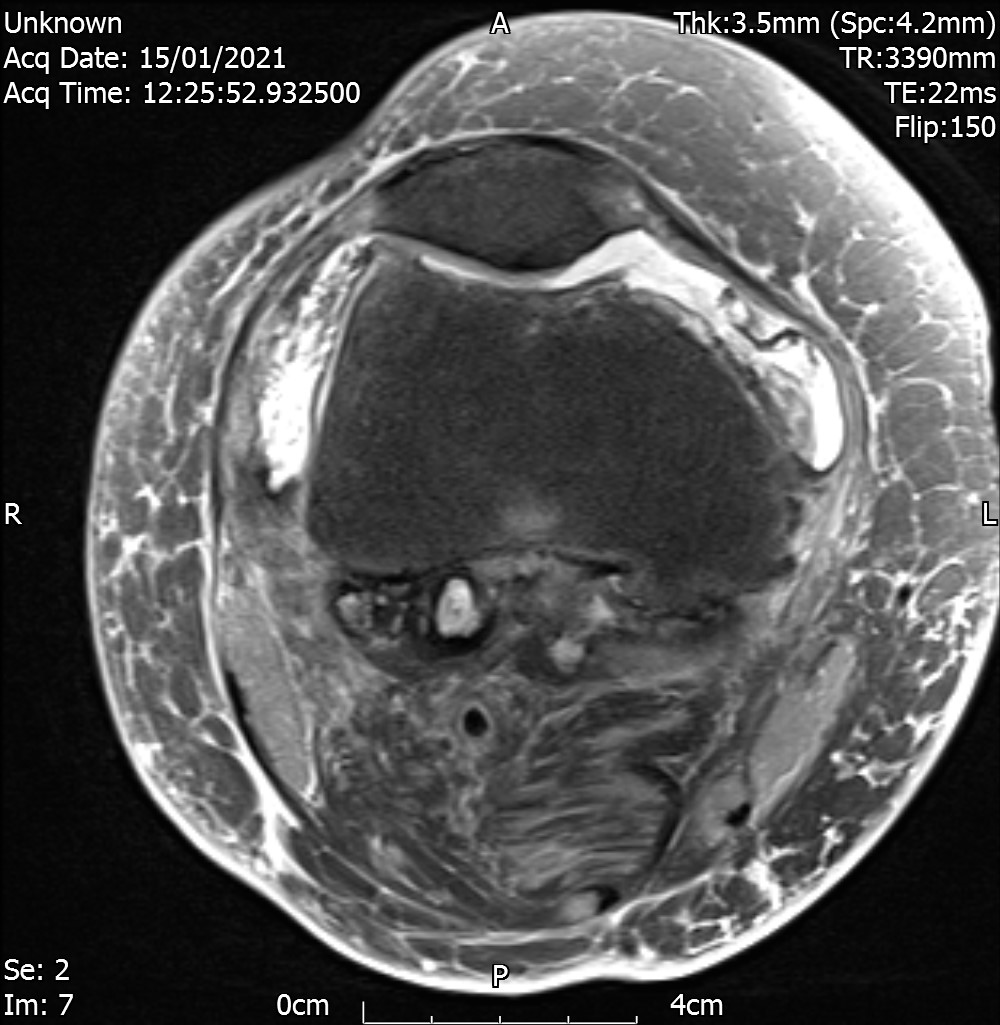
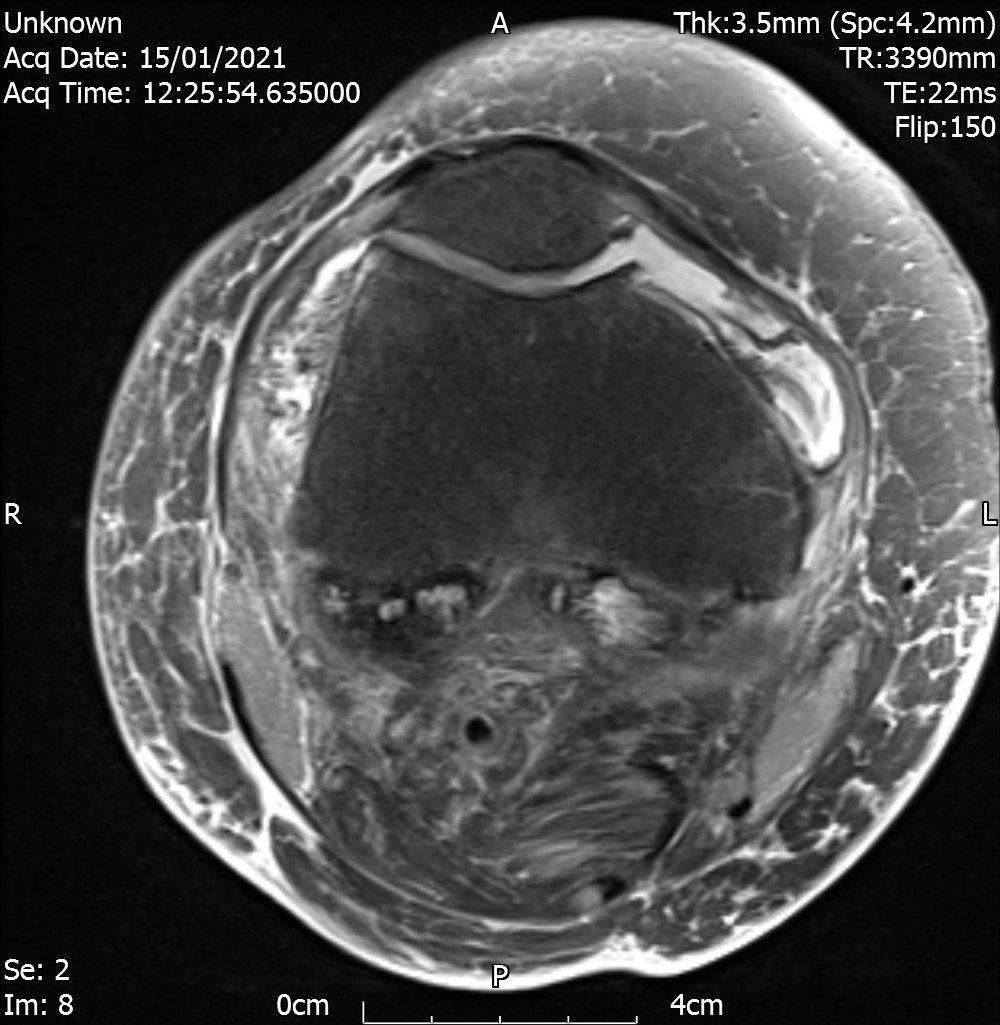
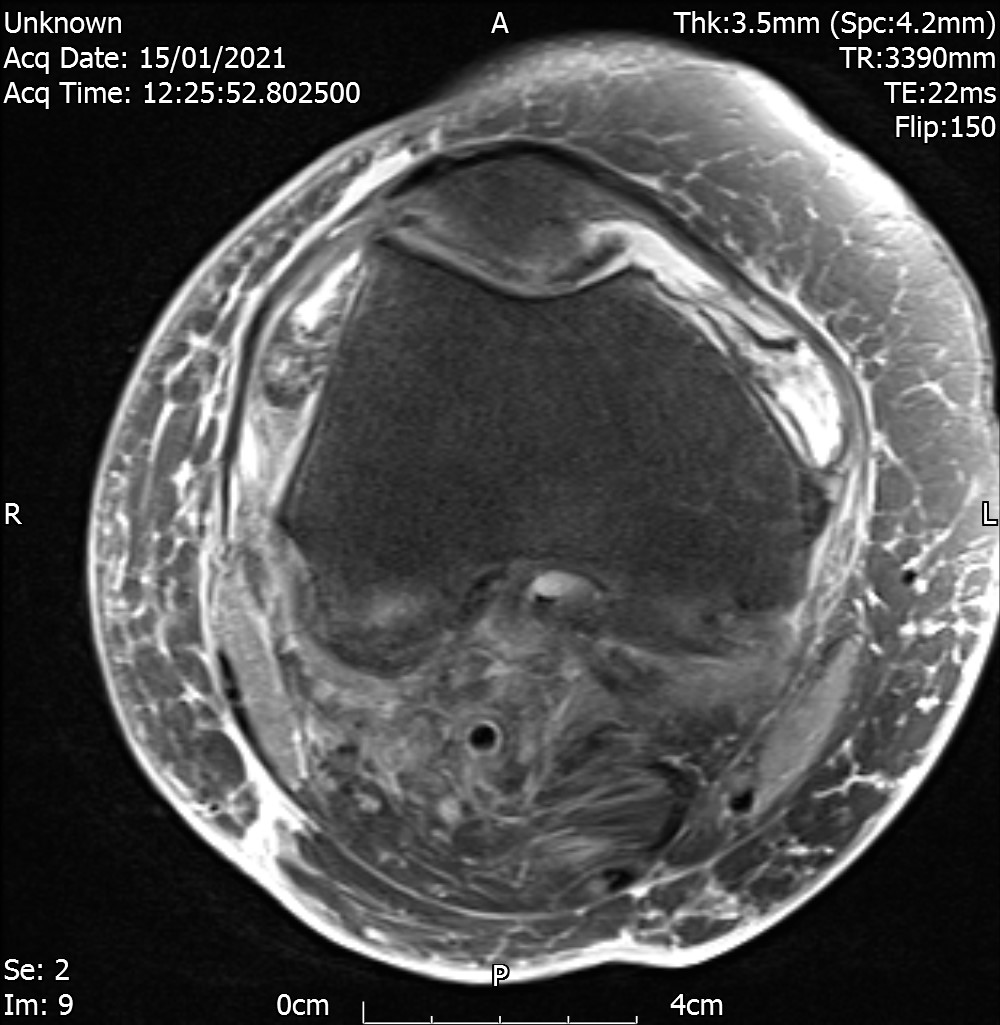
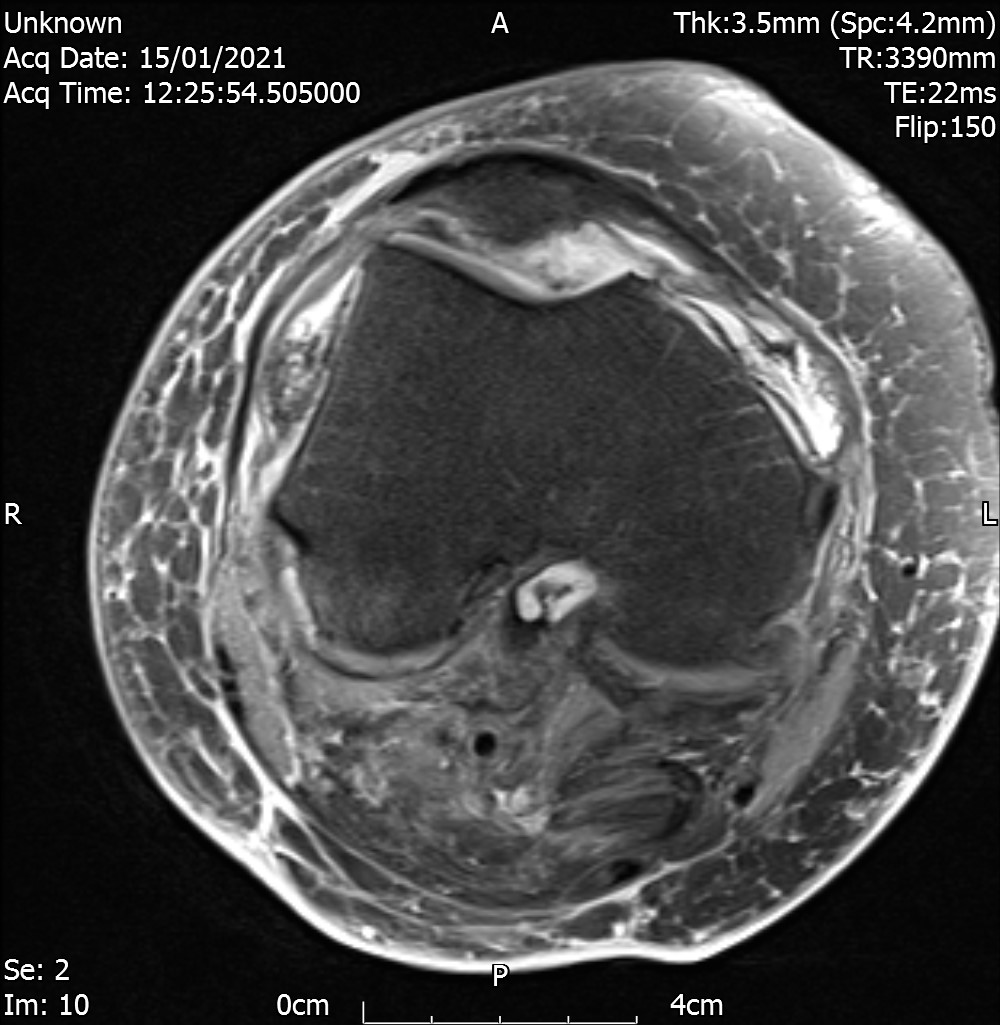
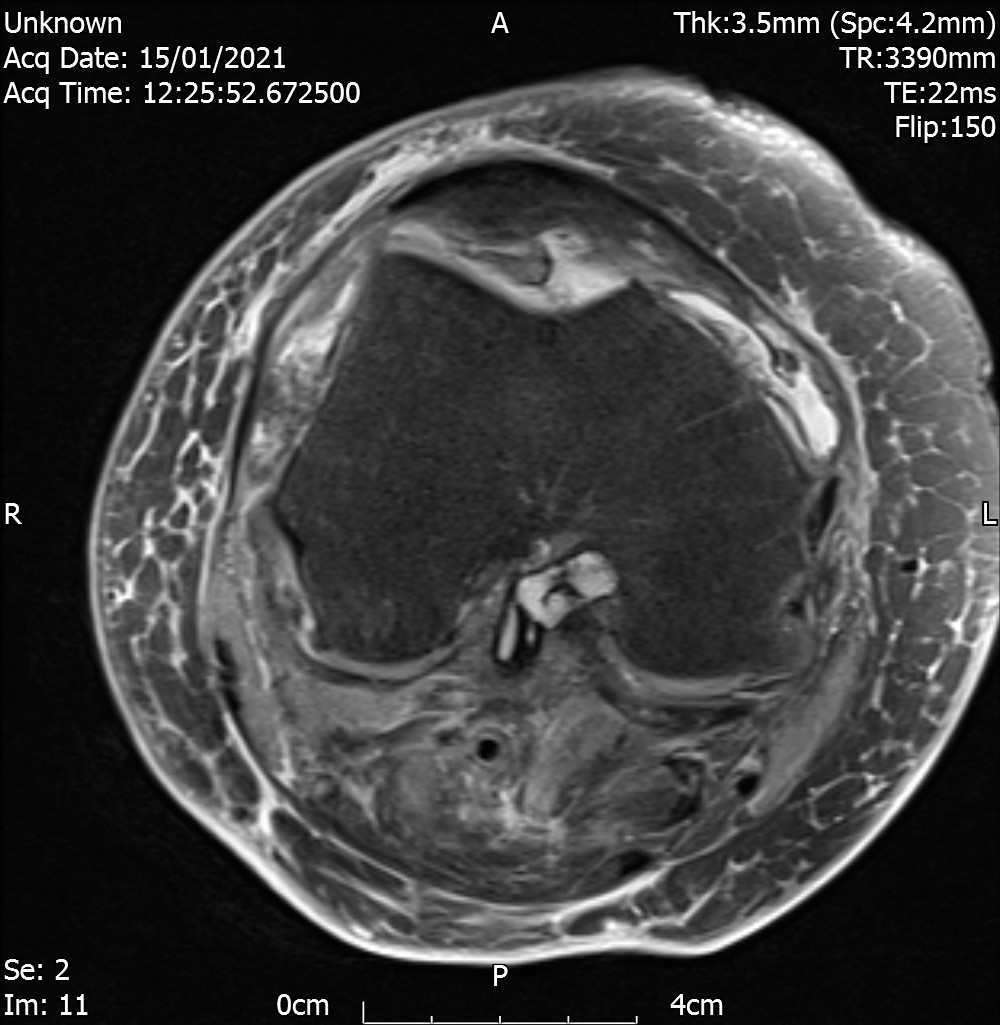
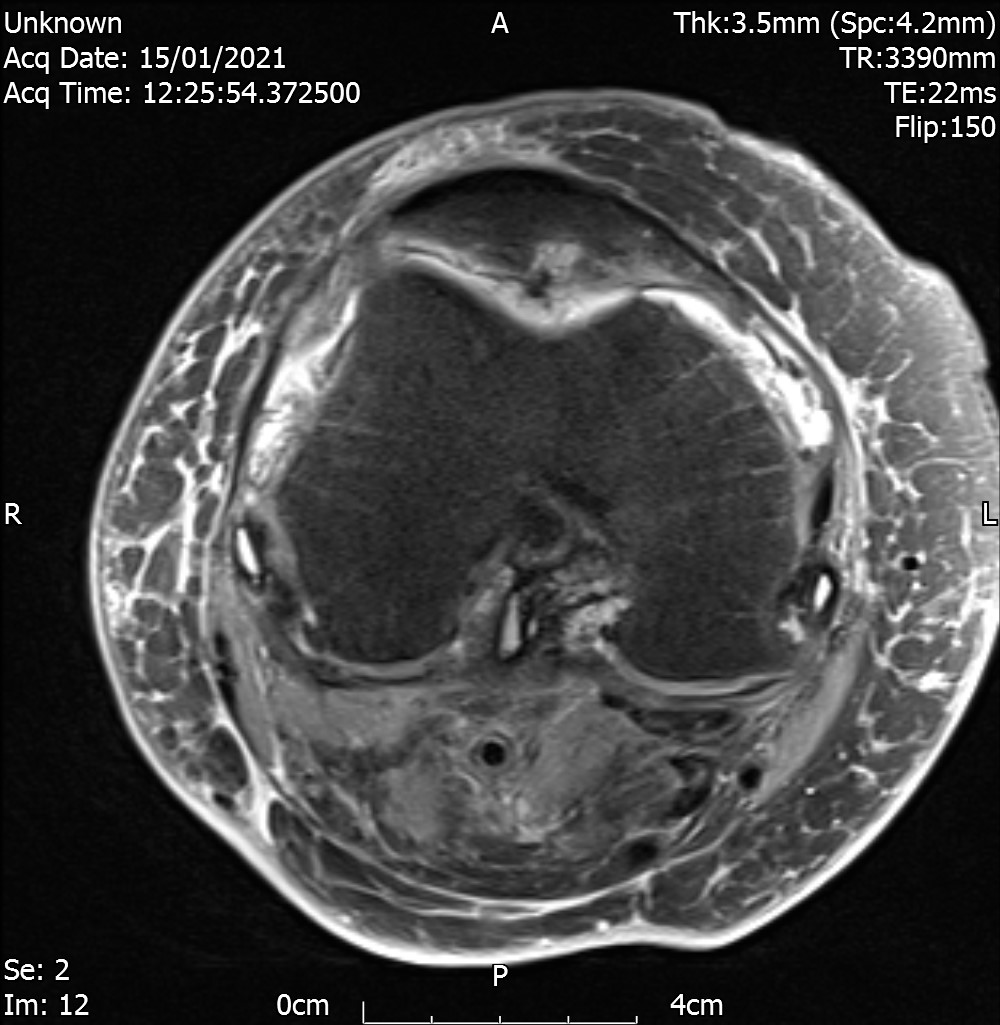
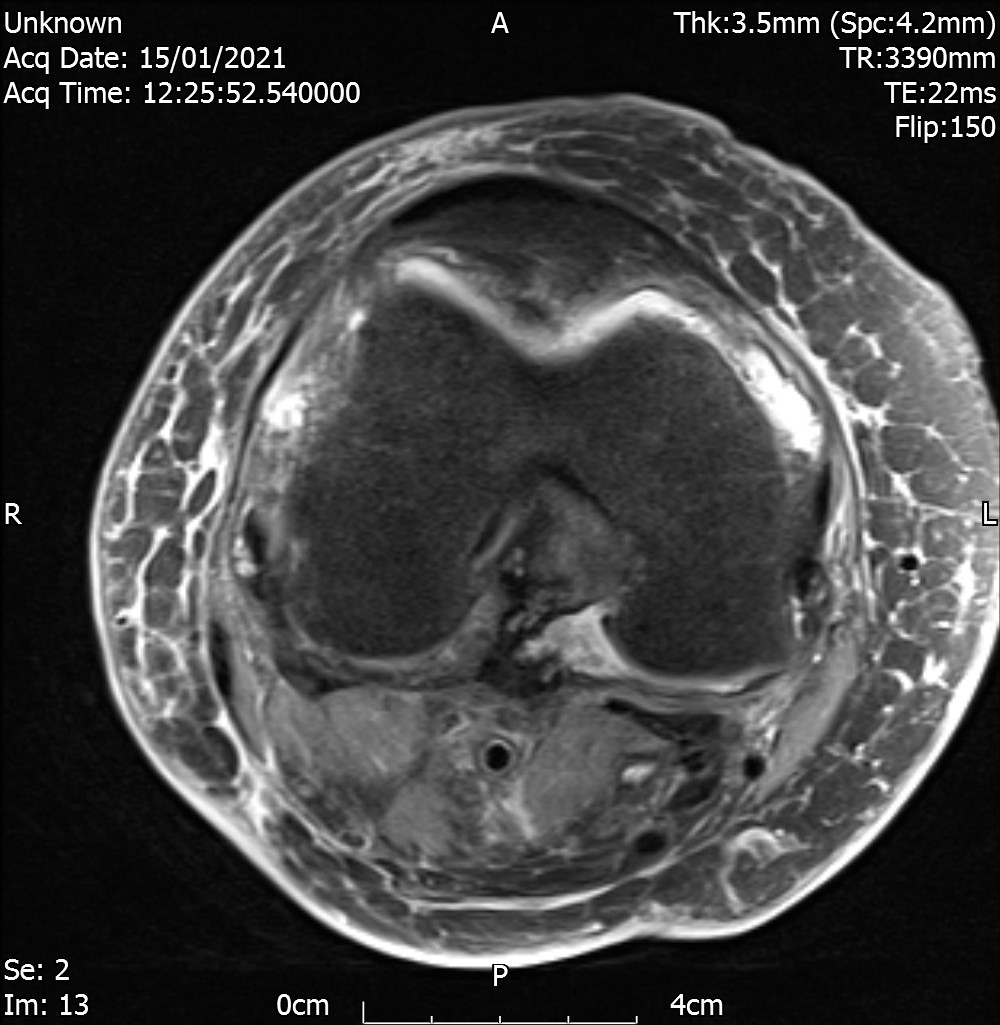
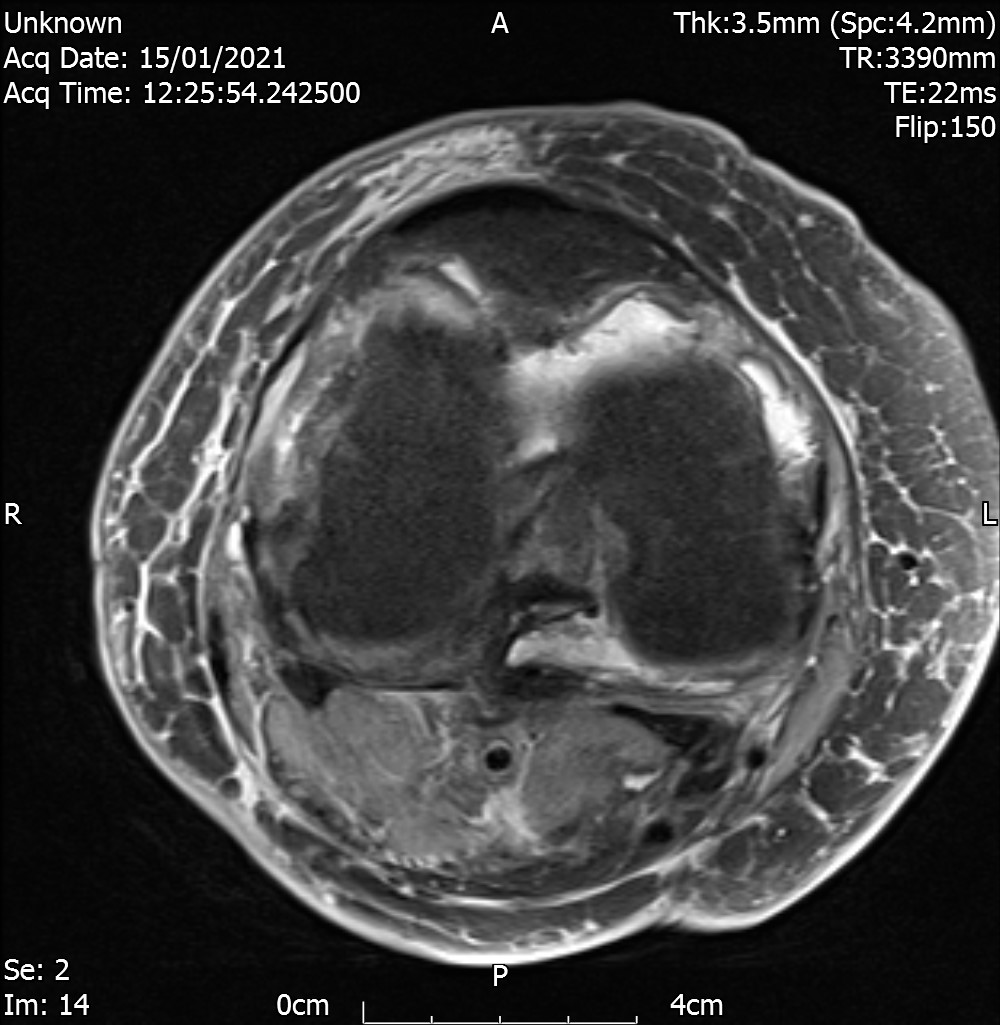
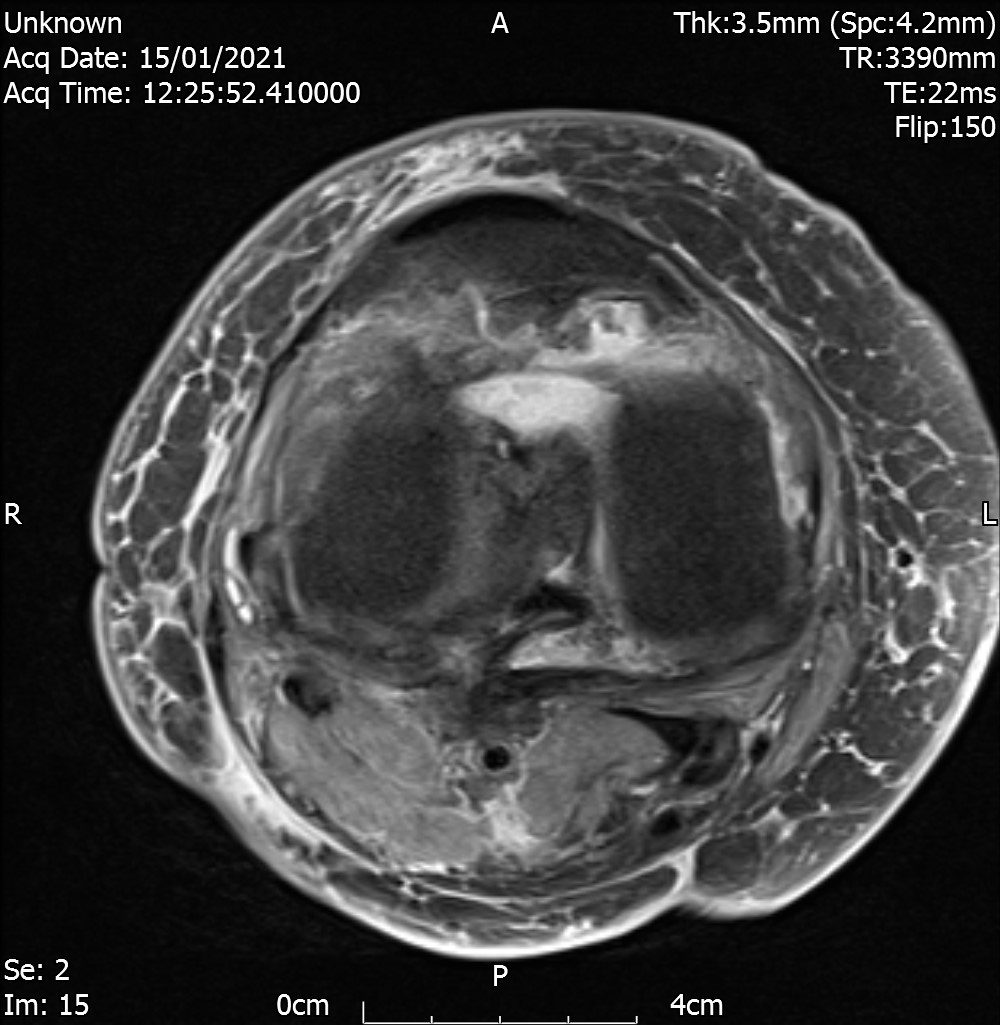
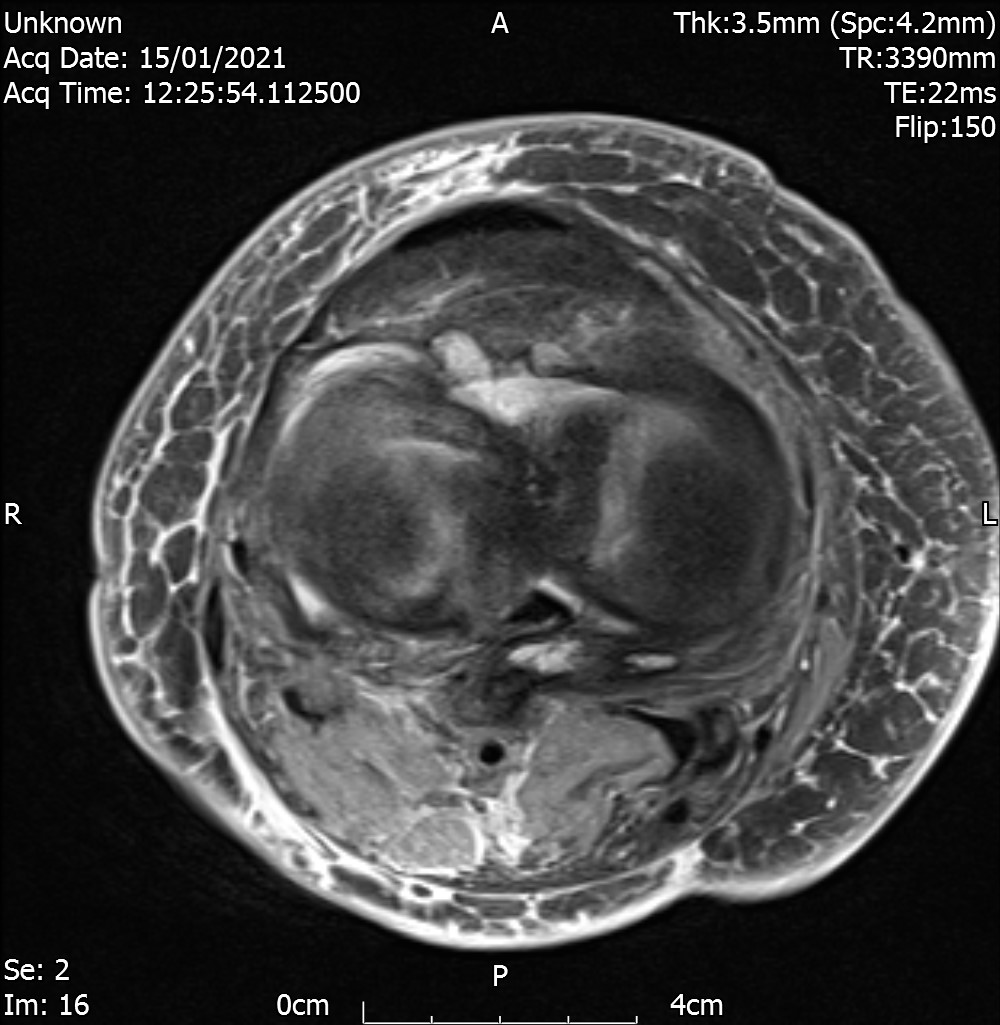
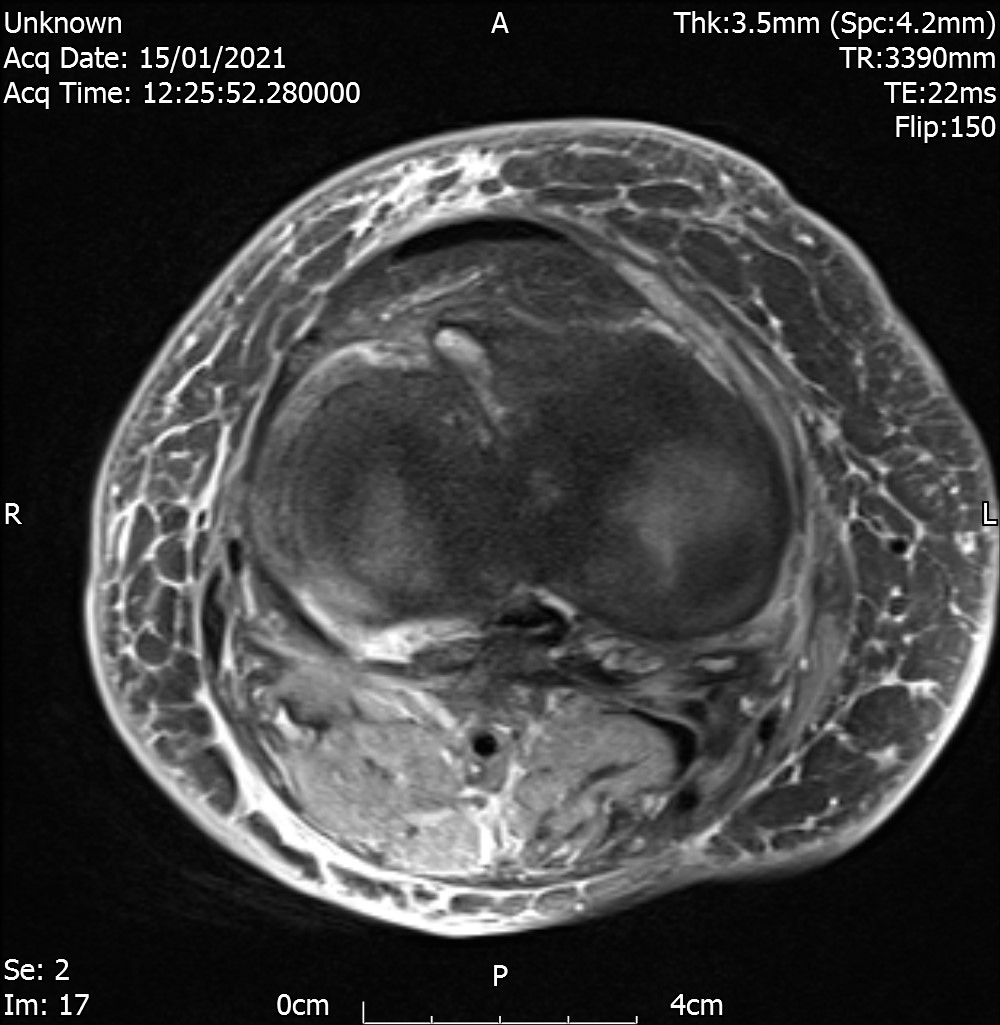
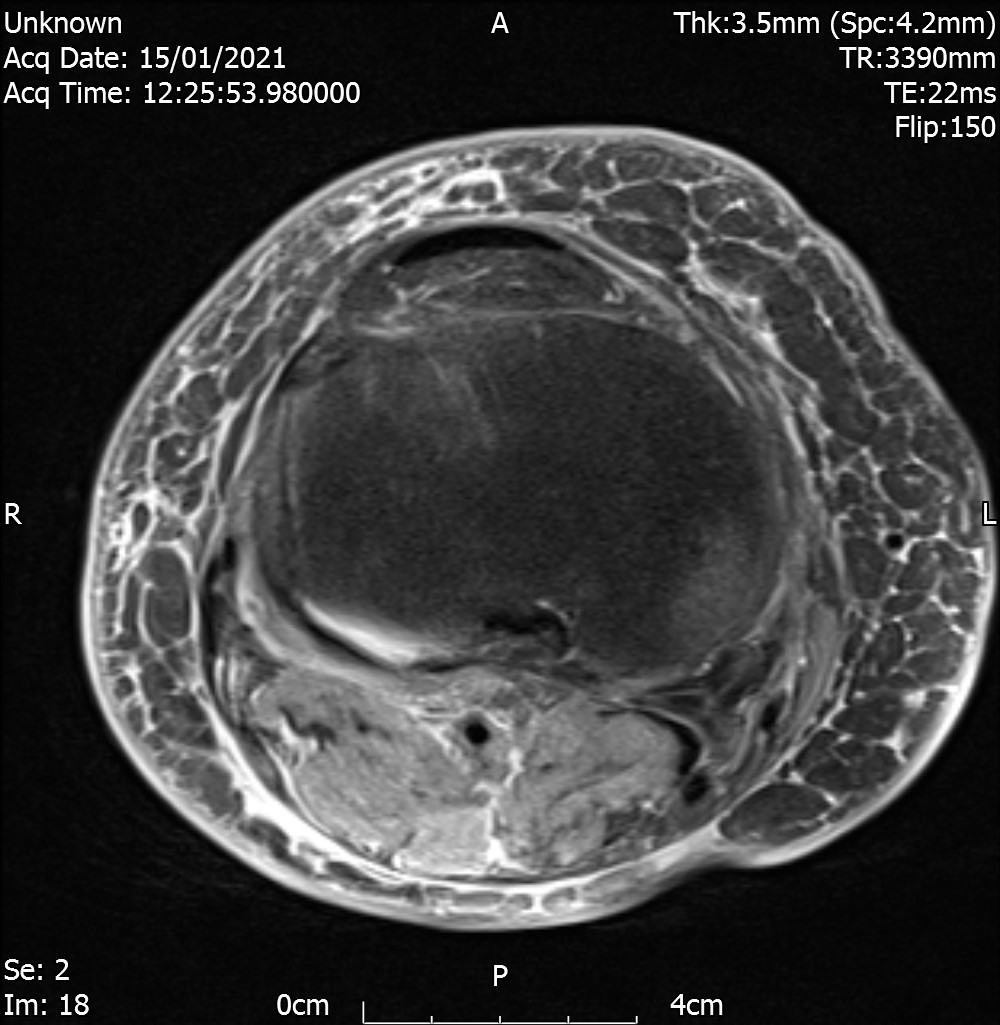
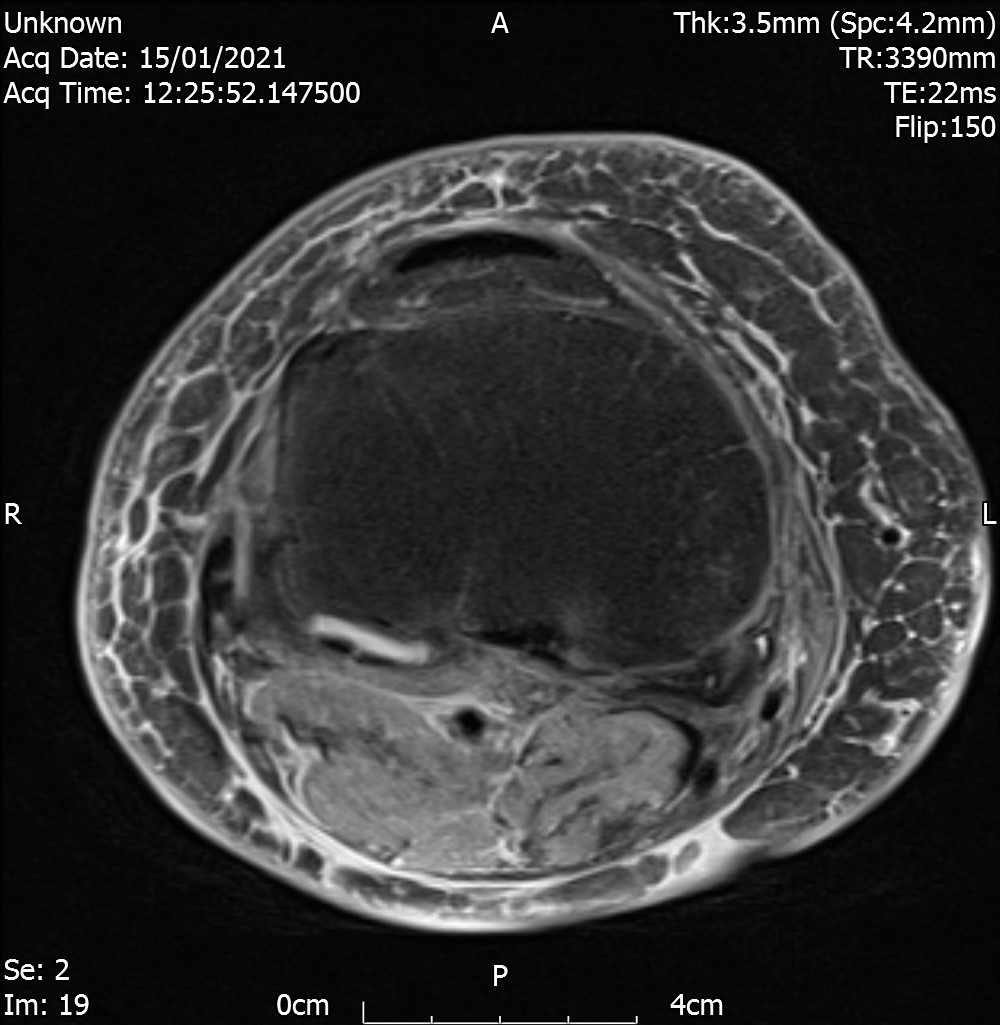
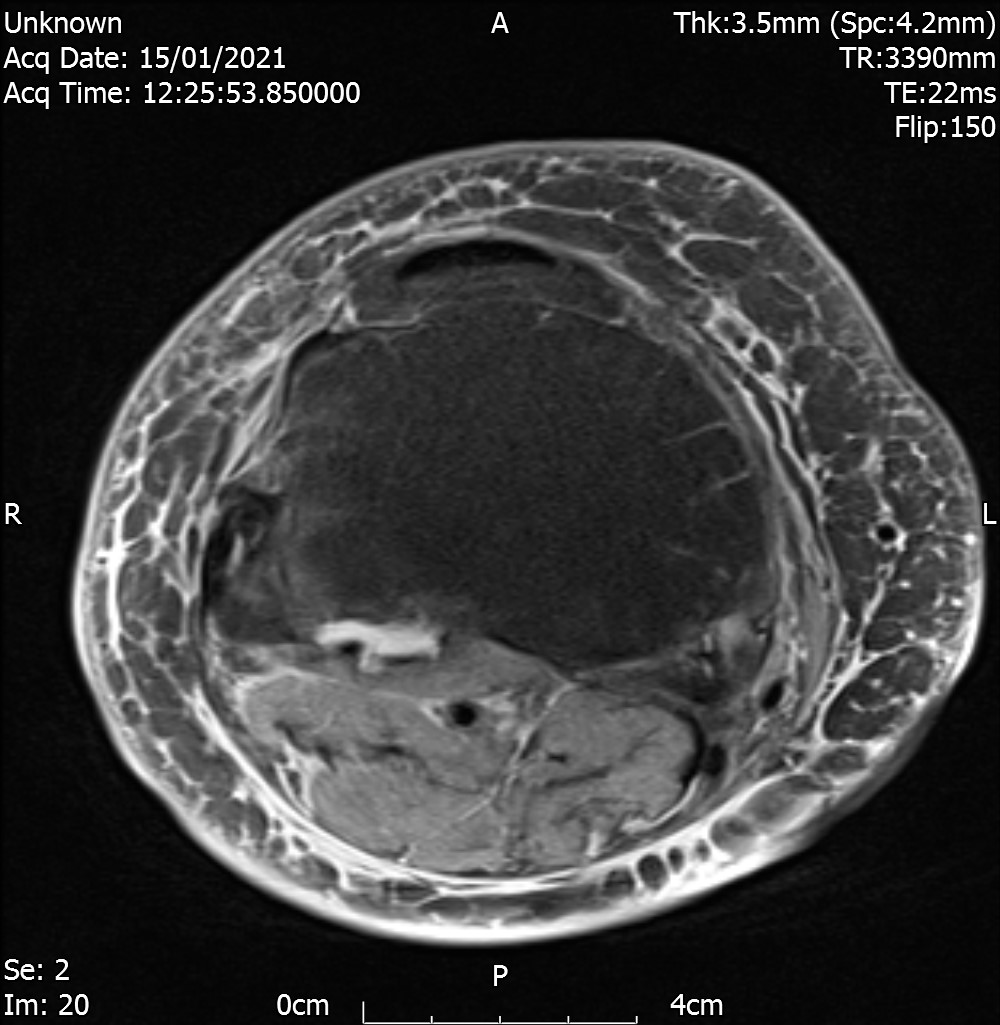
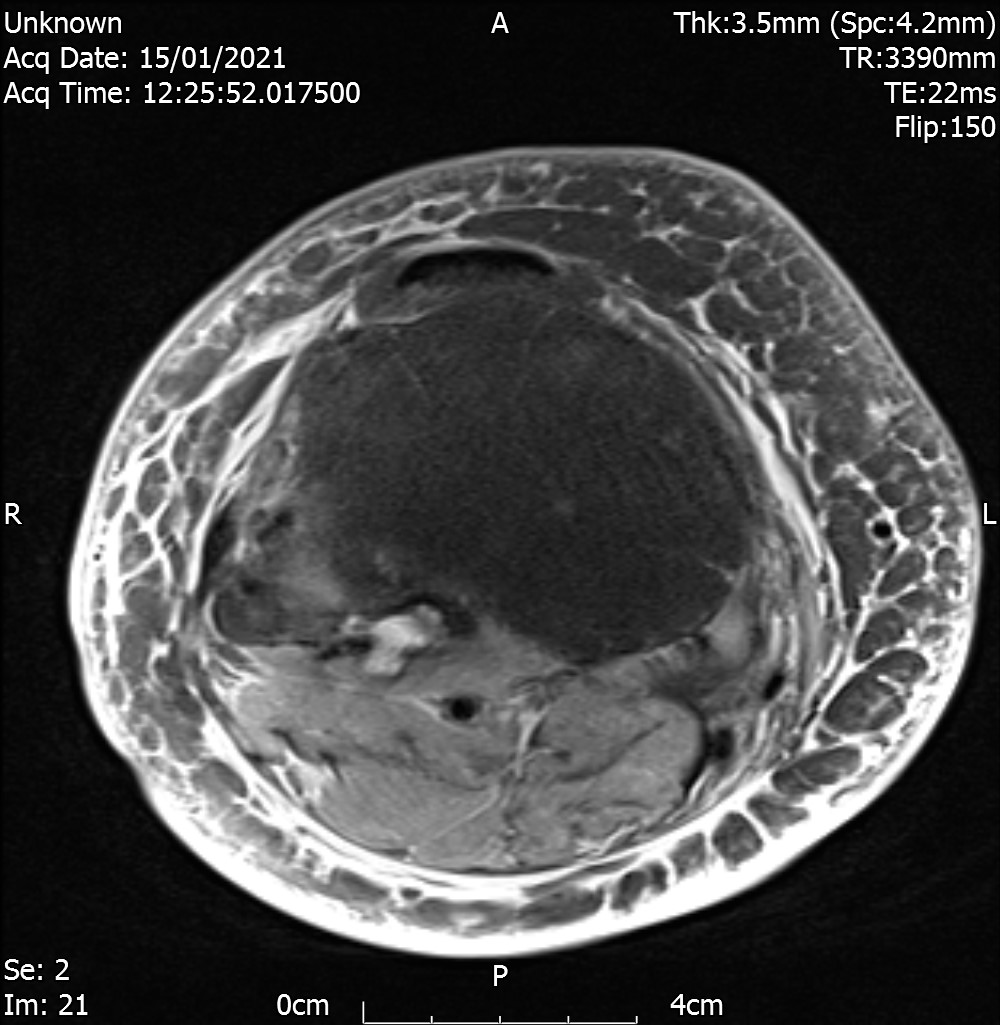
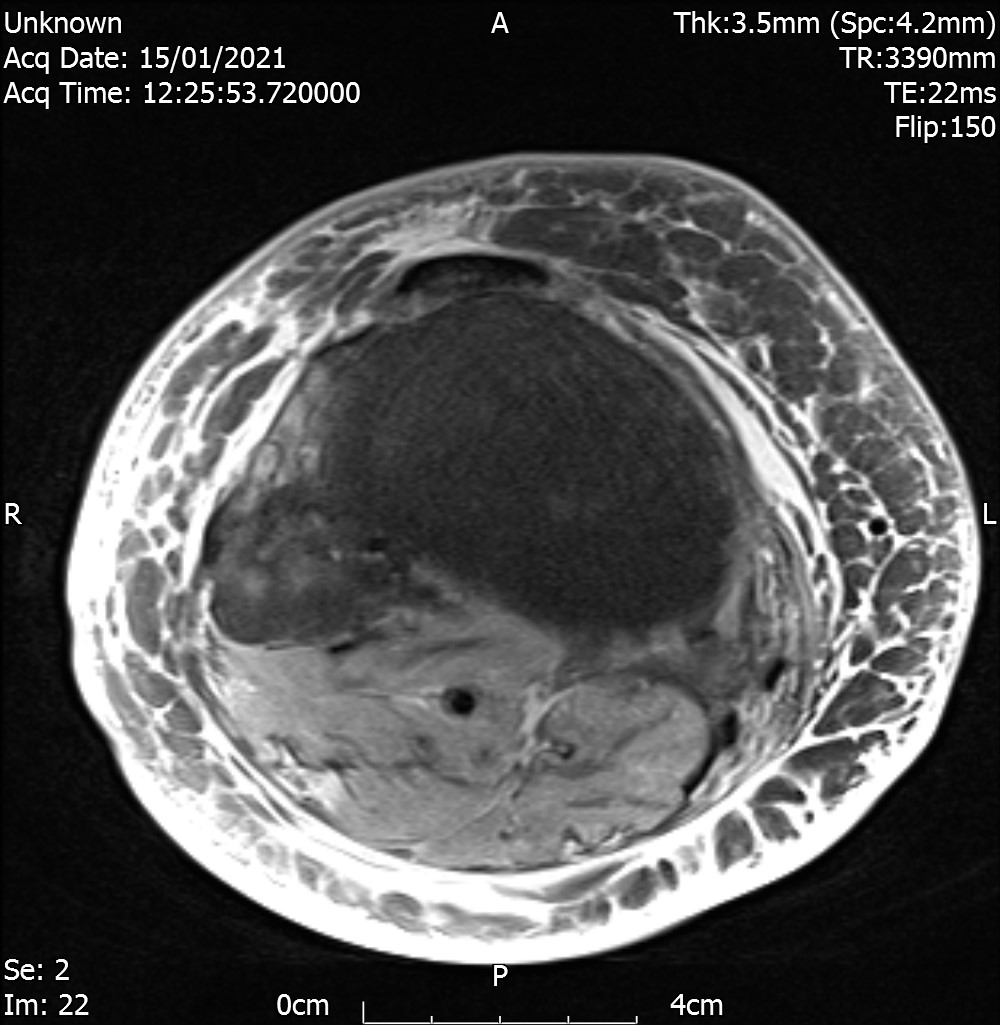
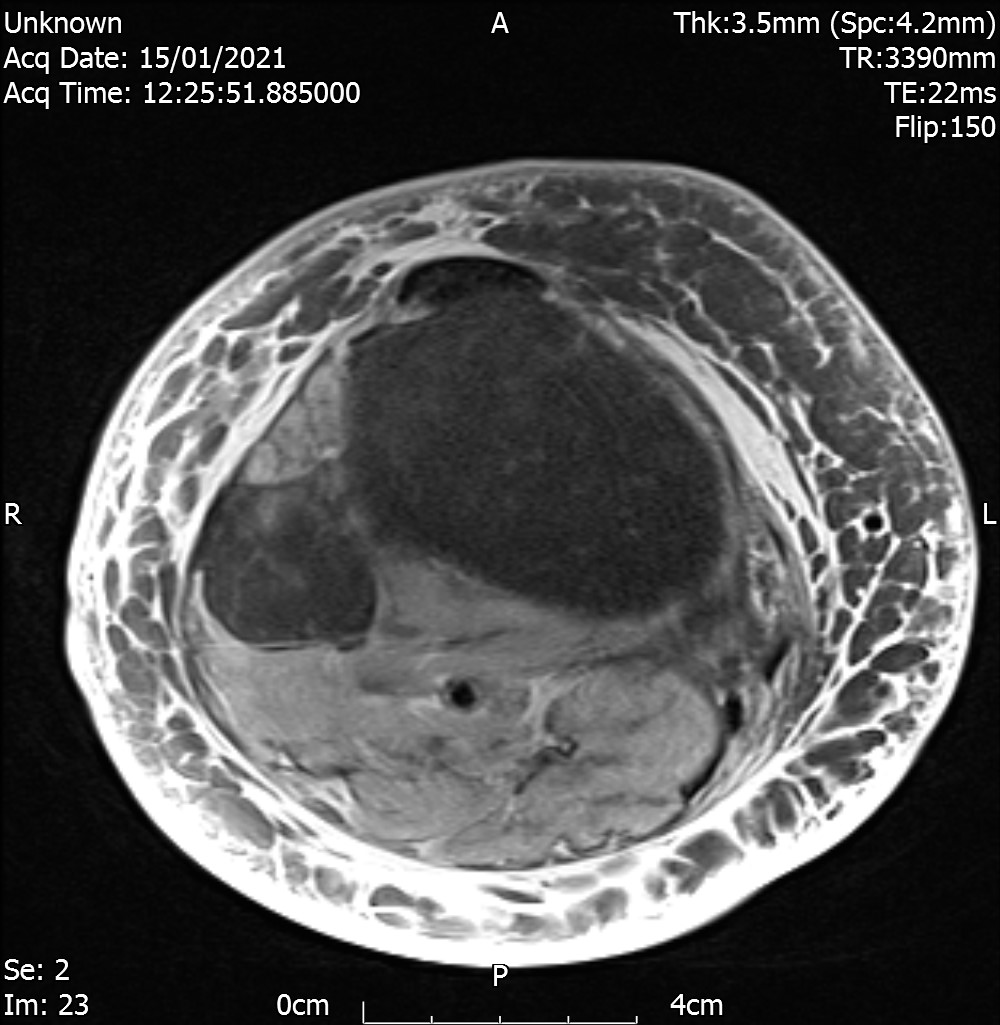
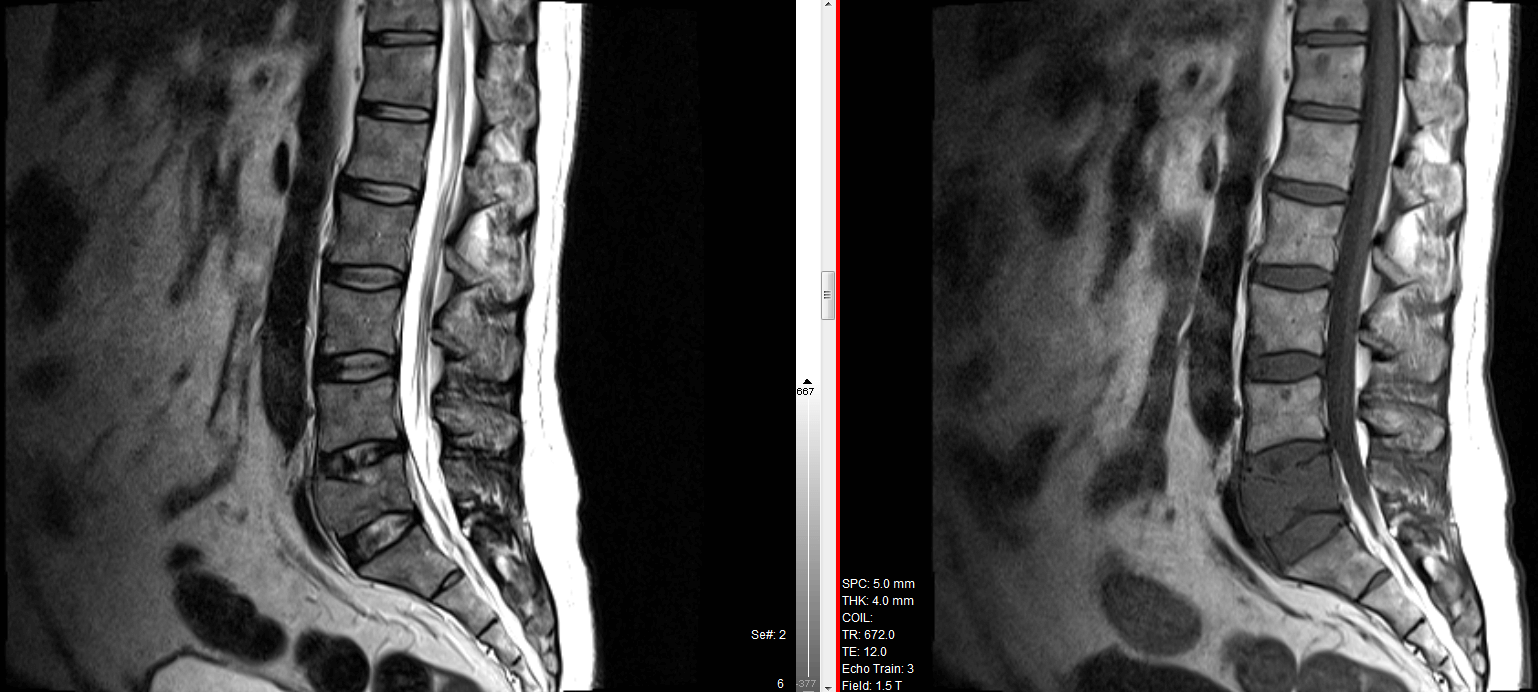
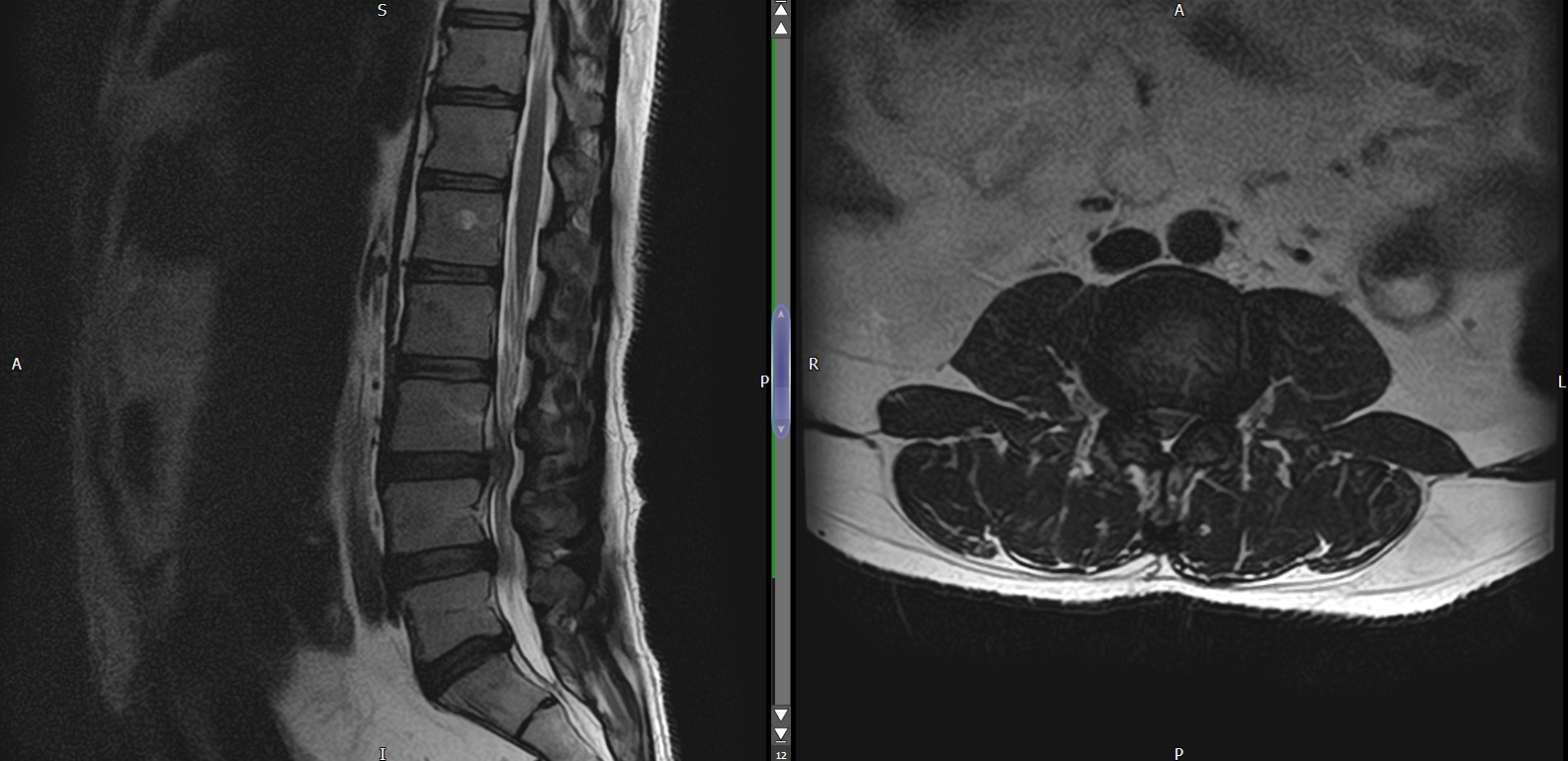
MRI
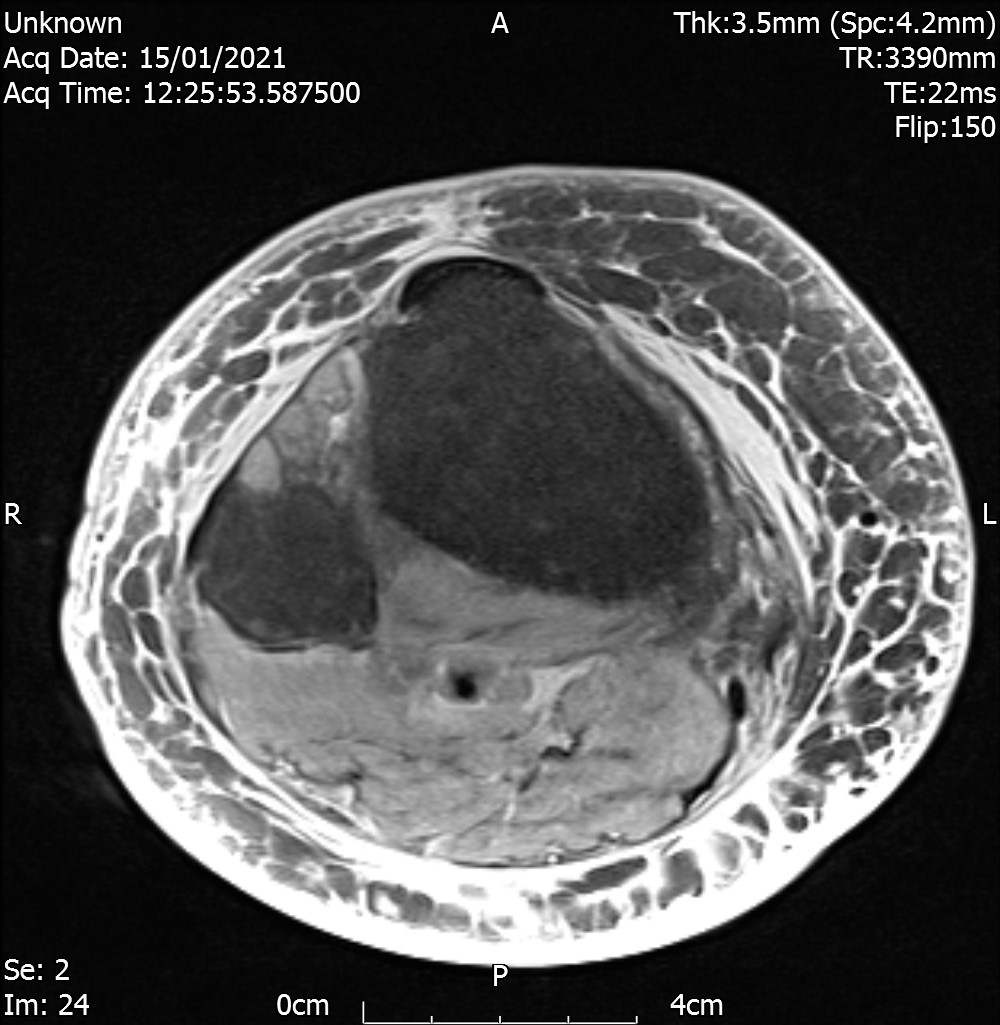
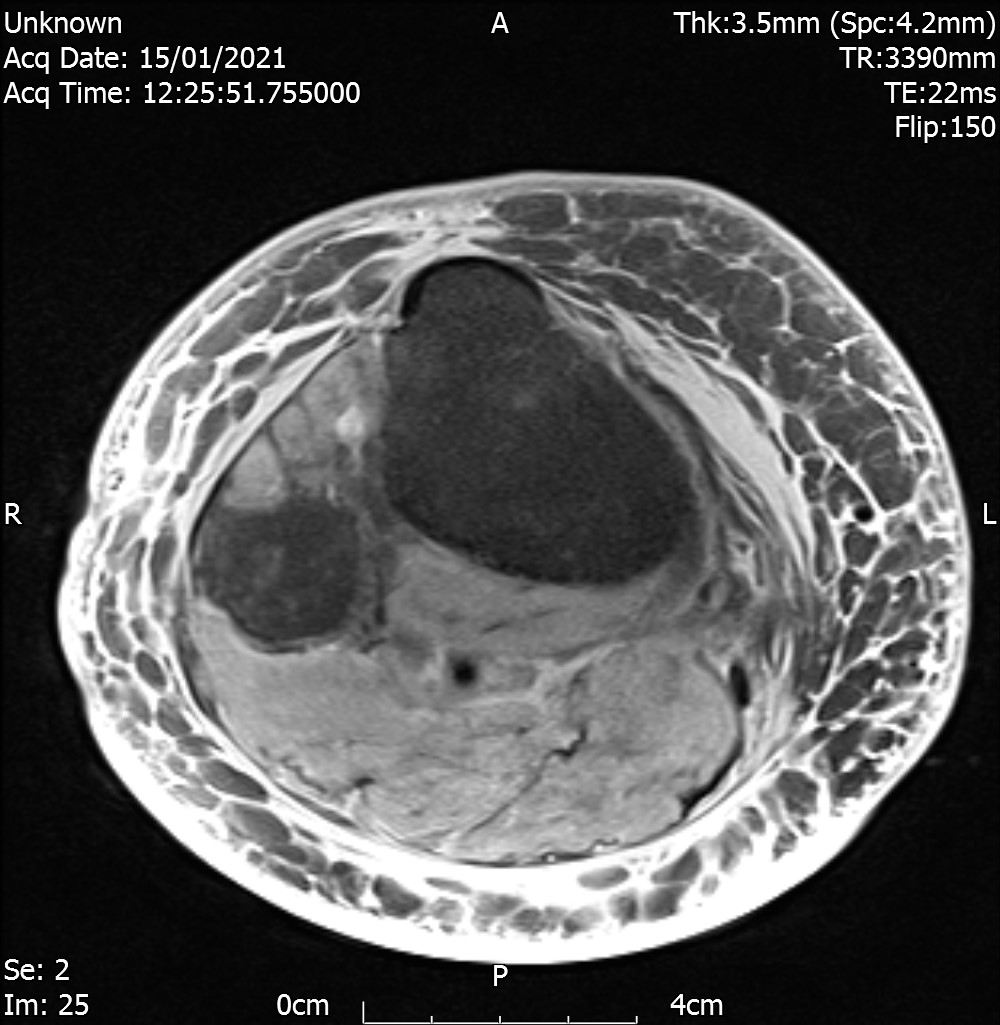
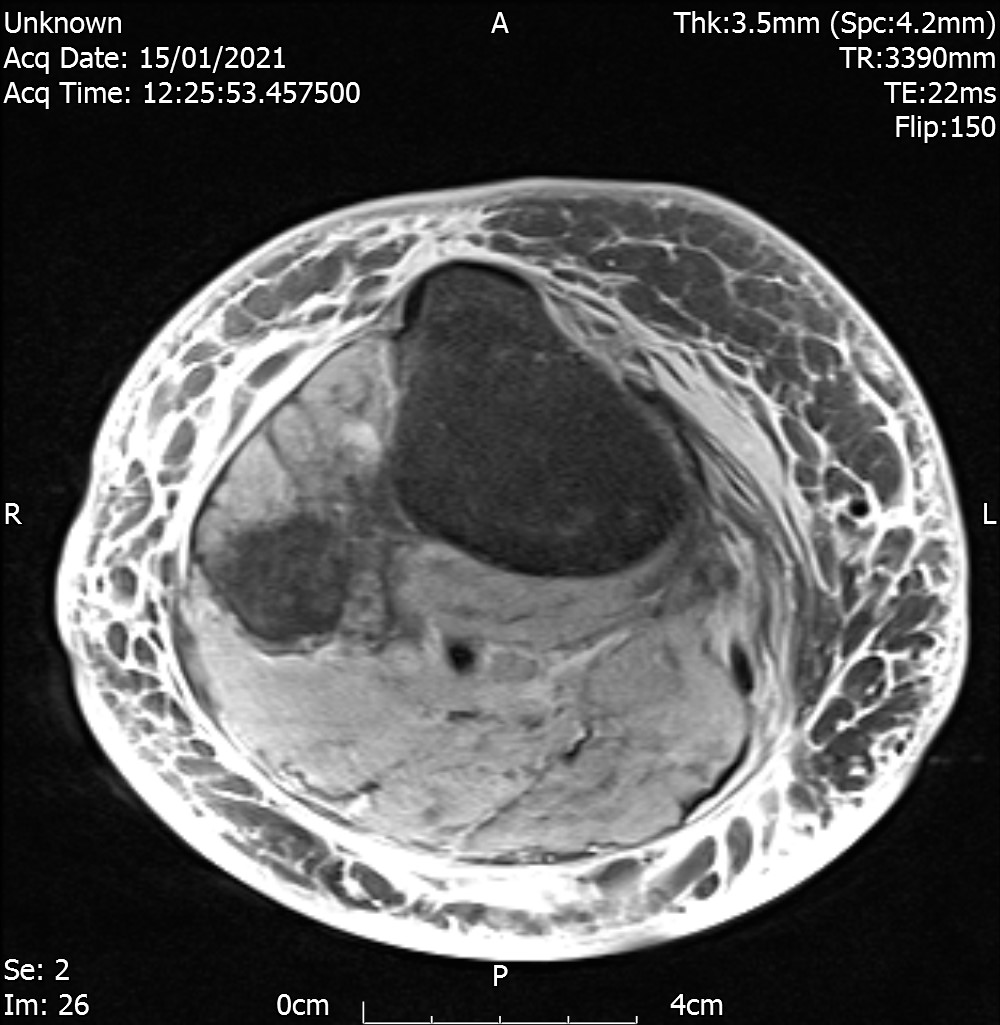
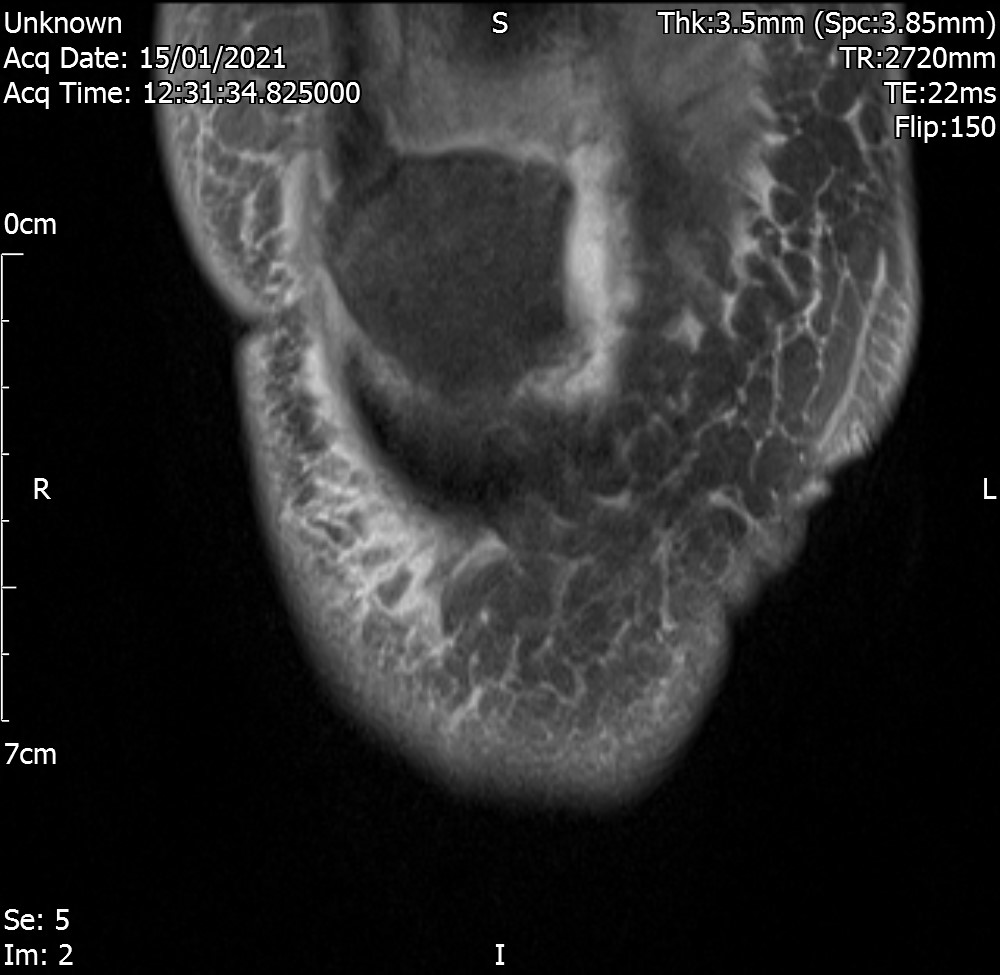
Axial view
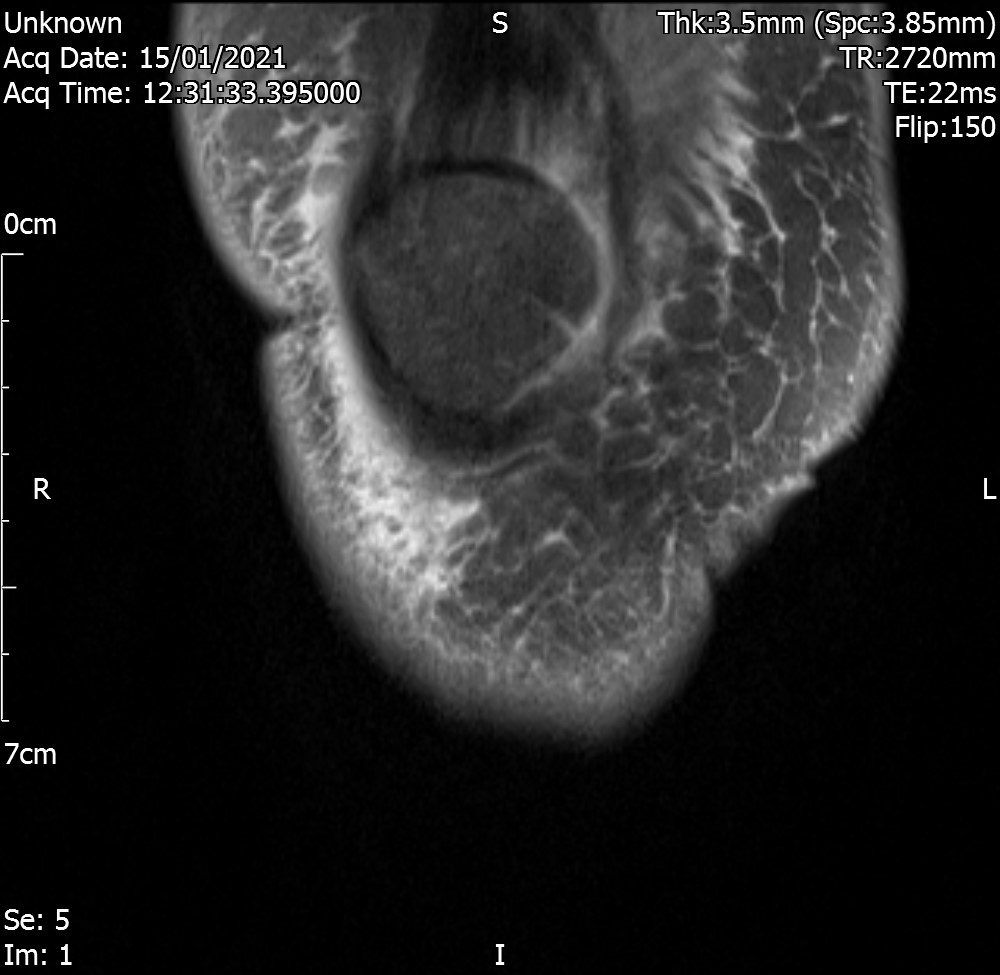
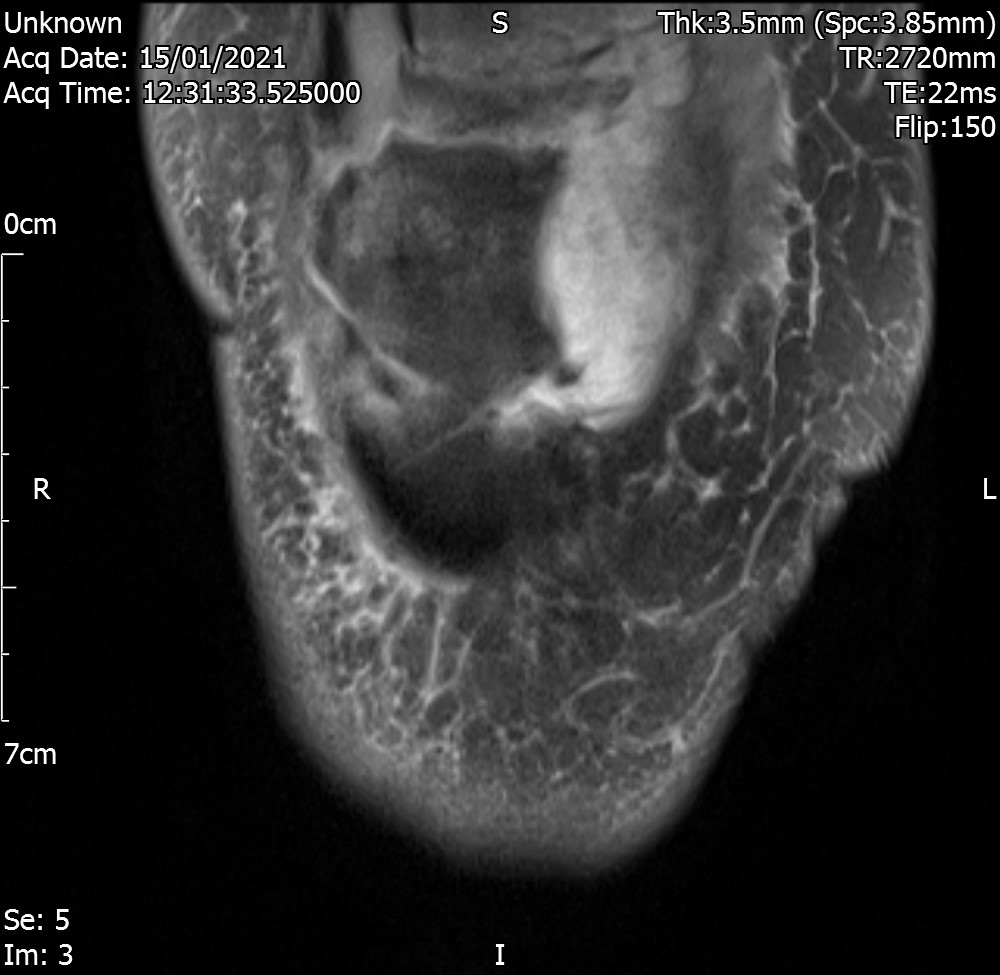
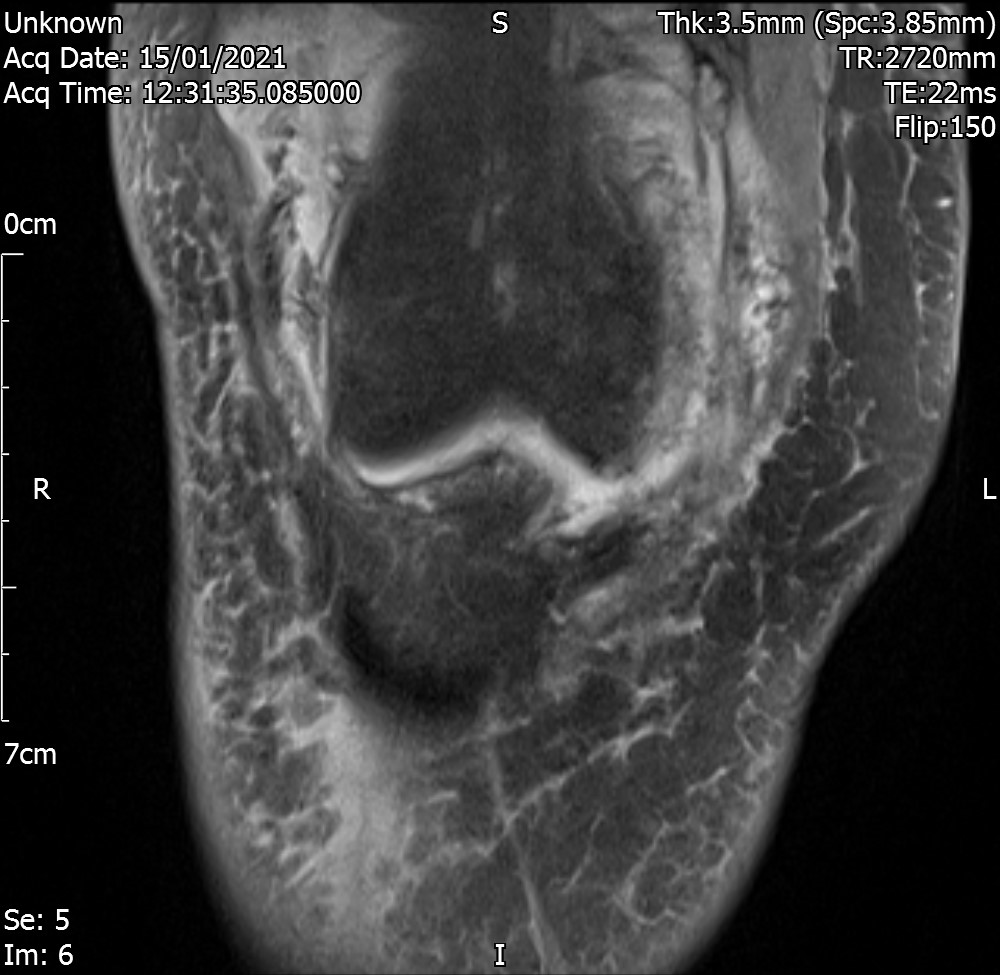
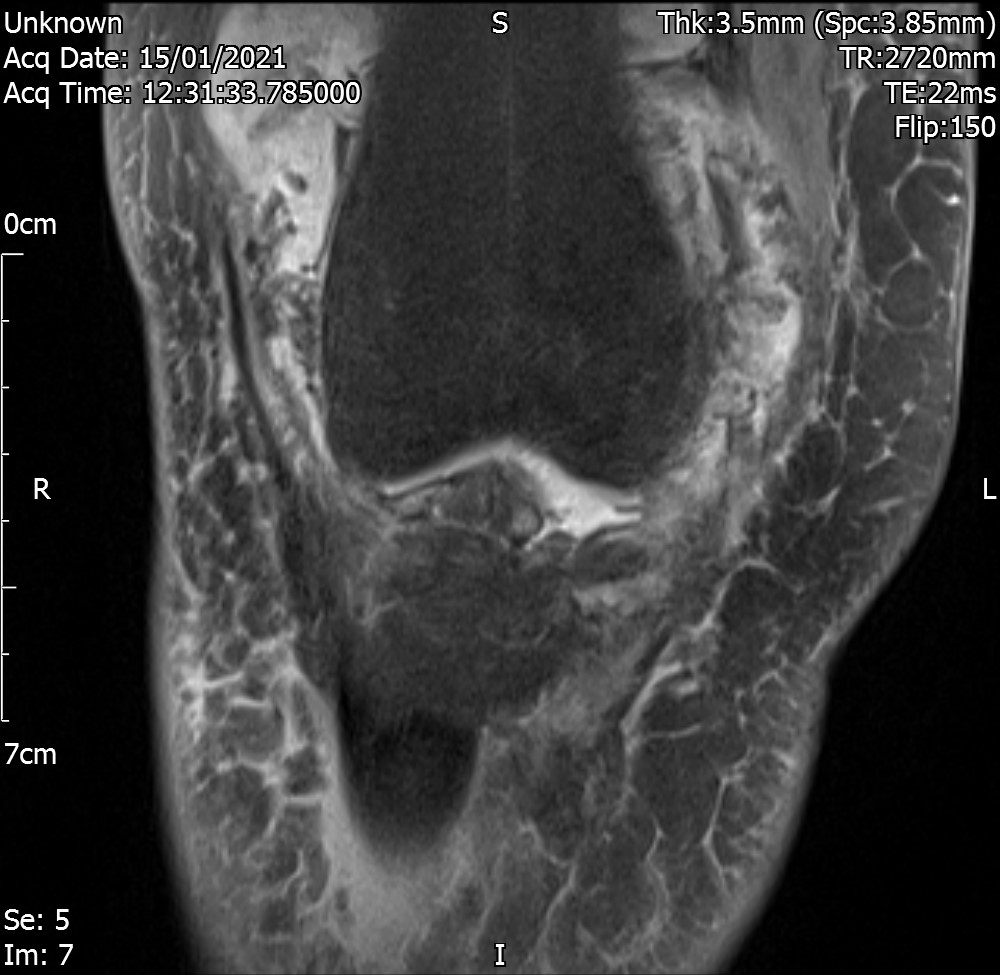
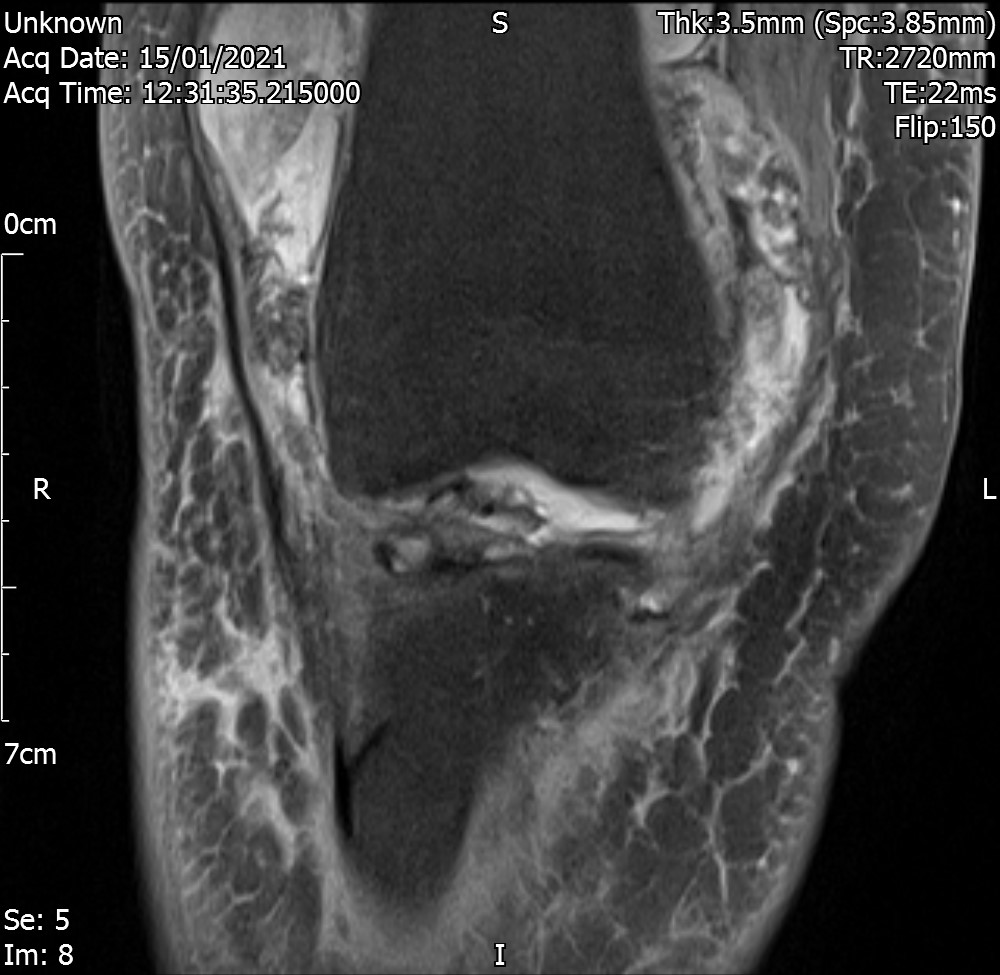
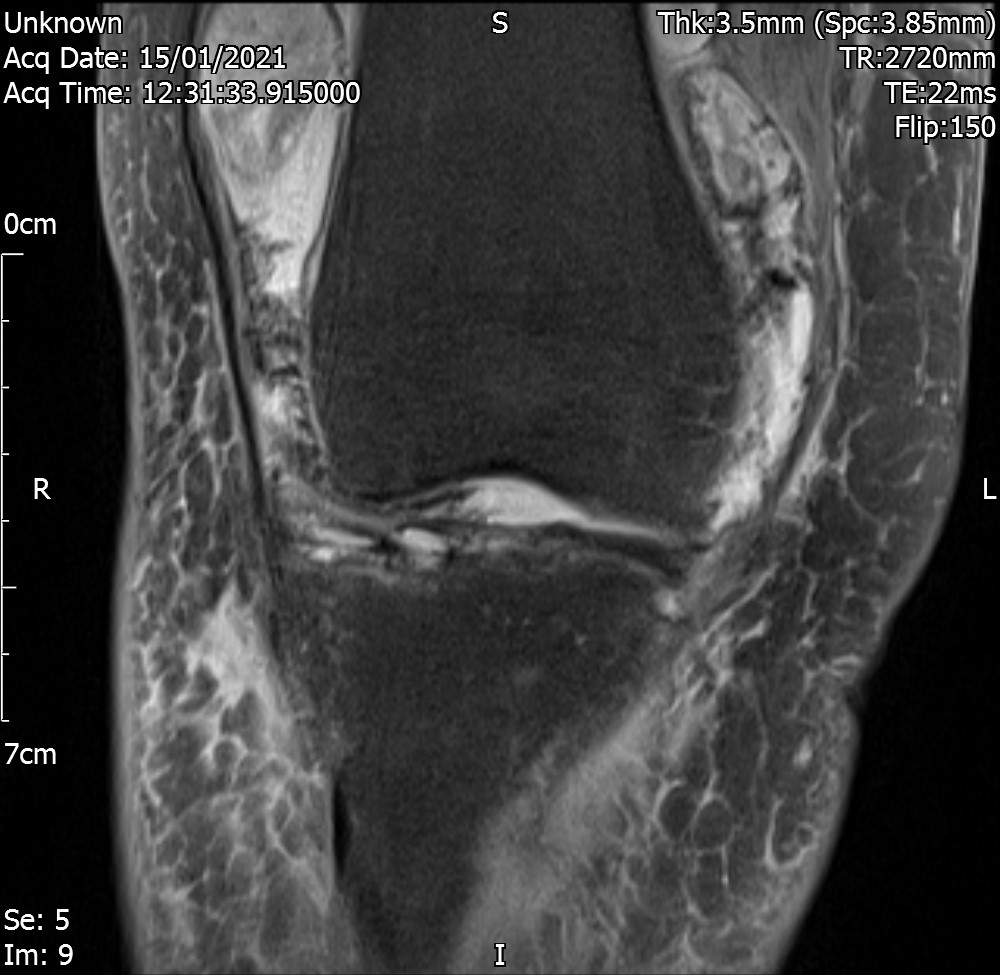
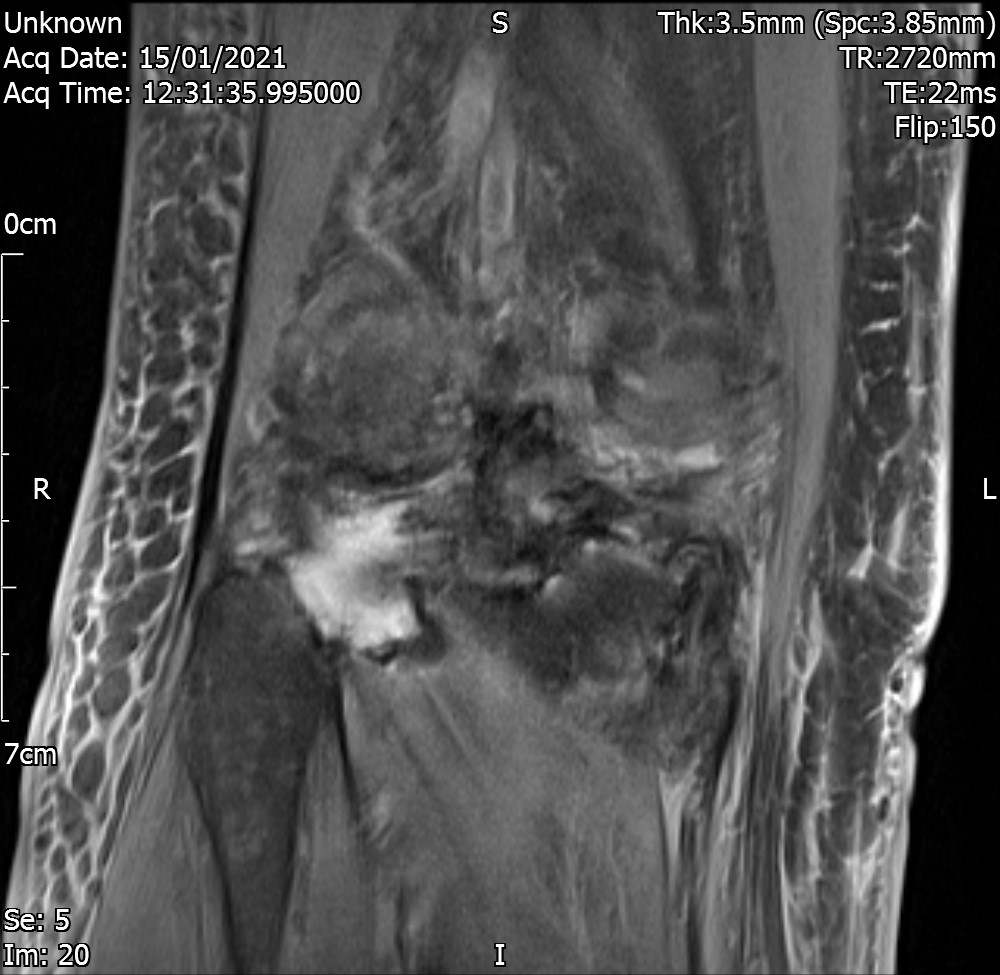
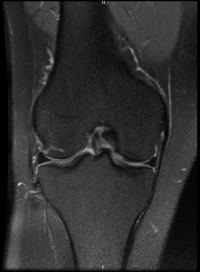
Coronal View – FS
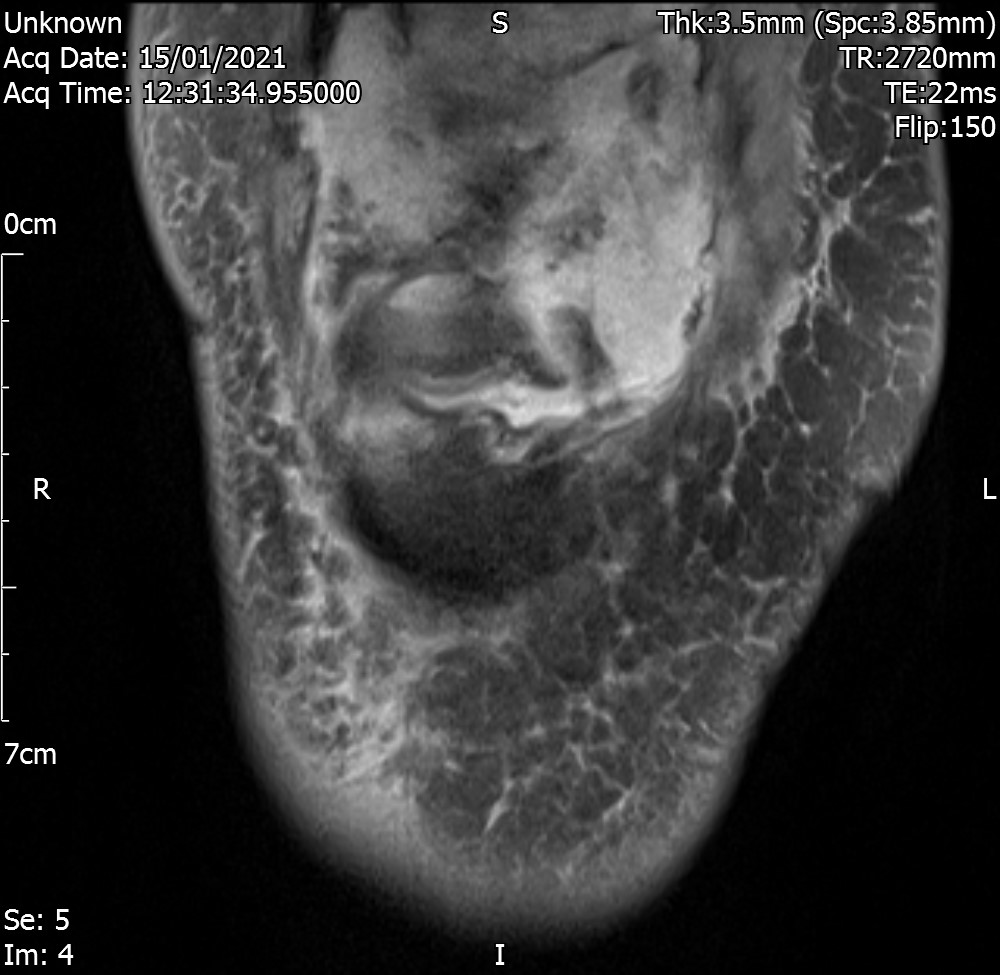
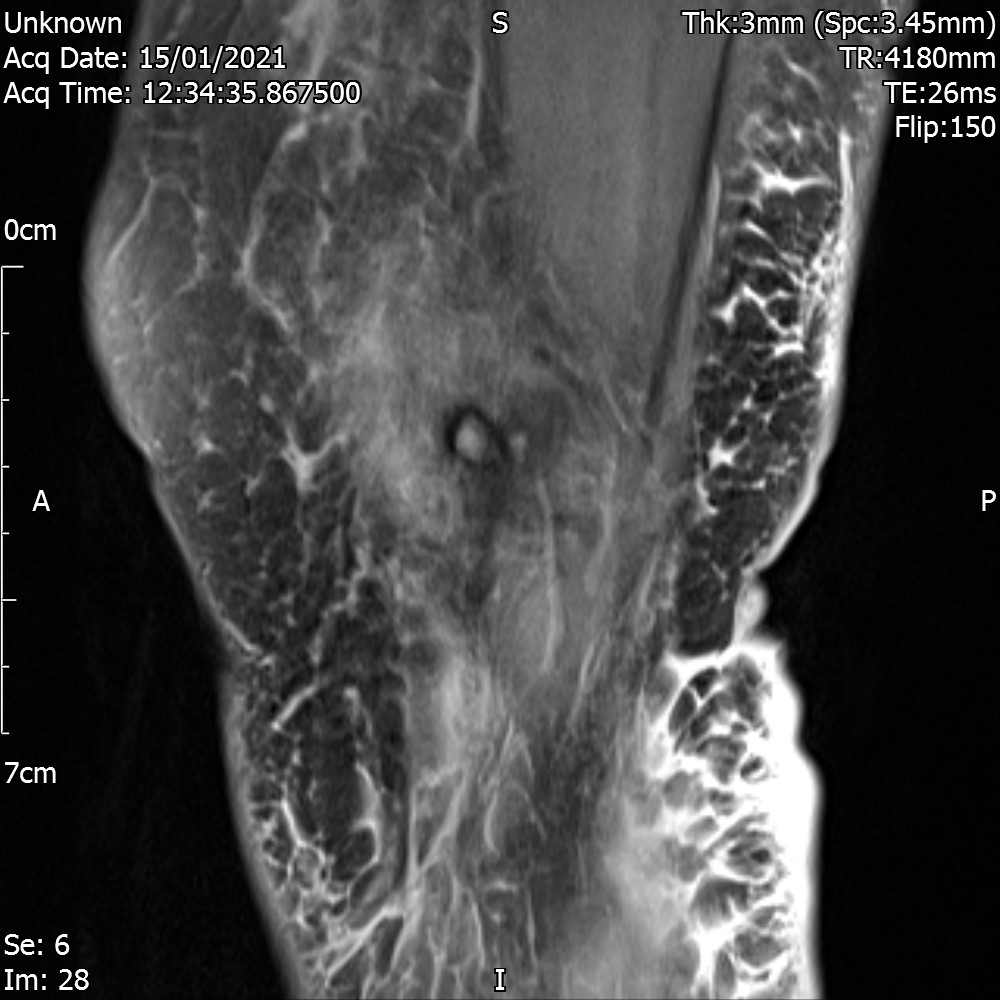
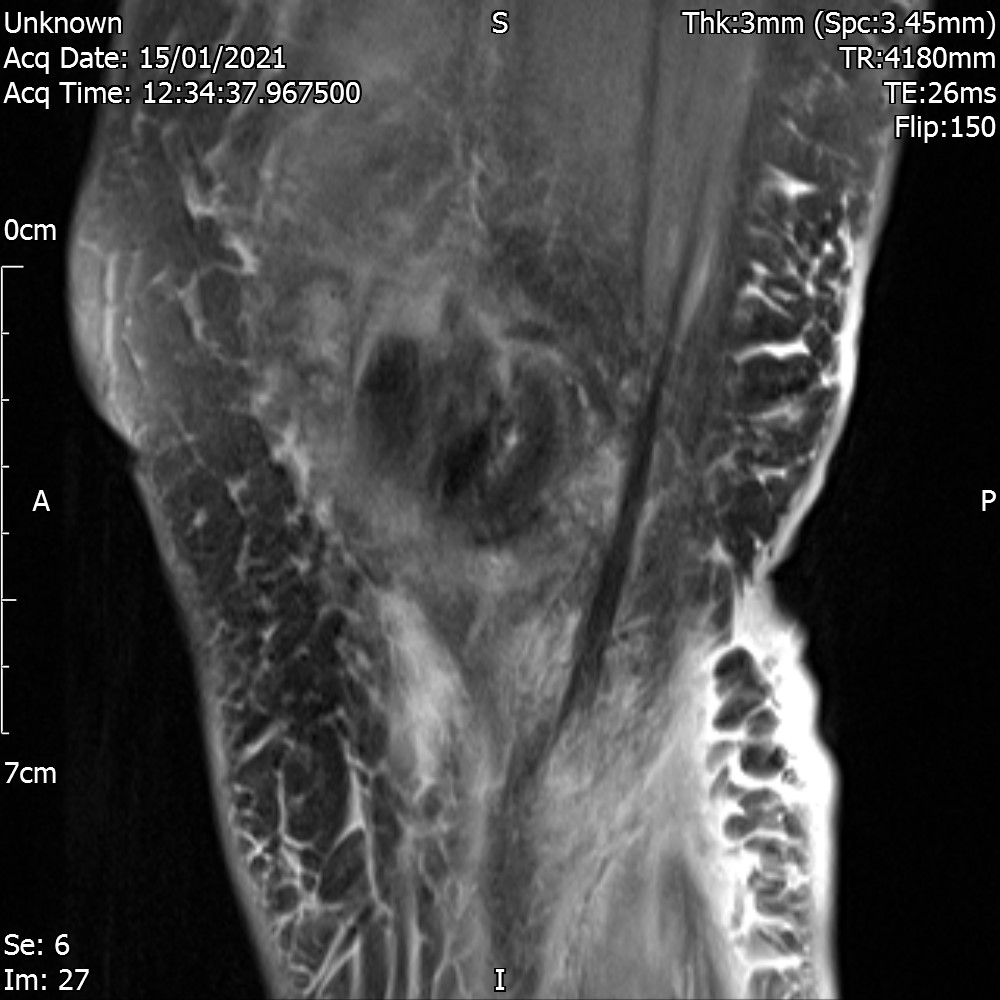
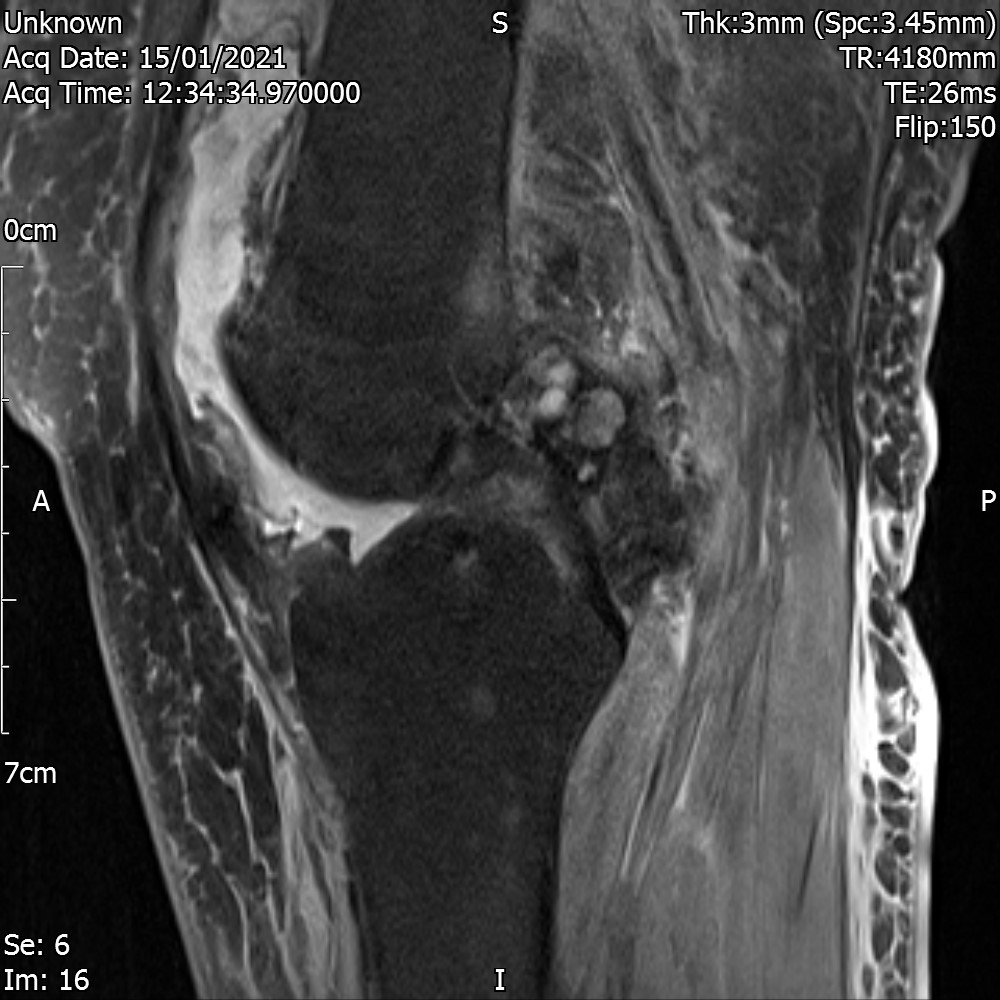
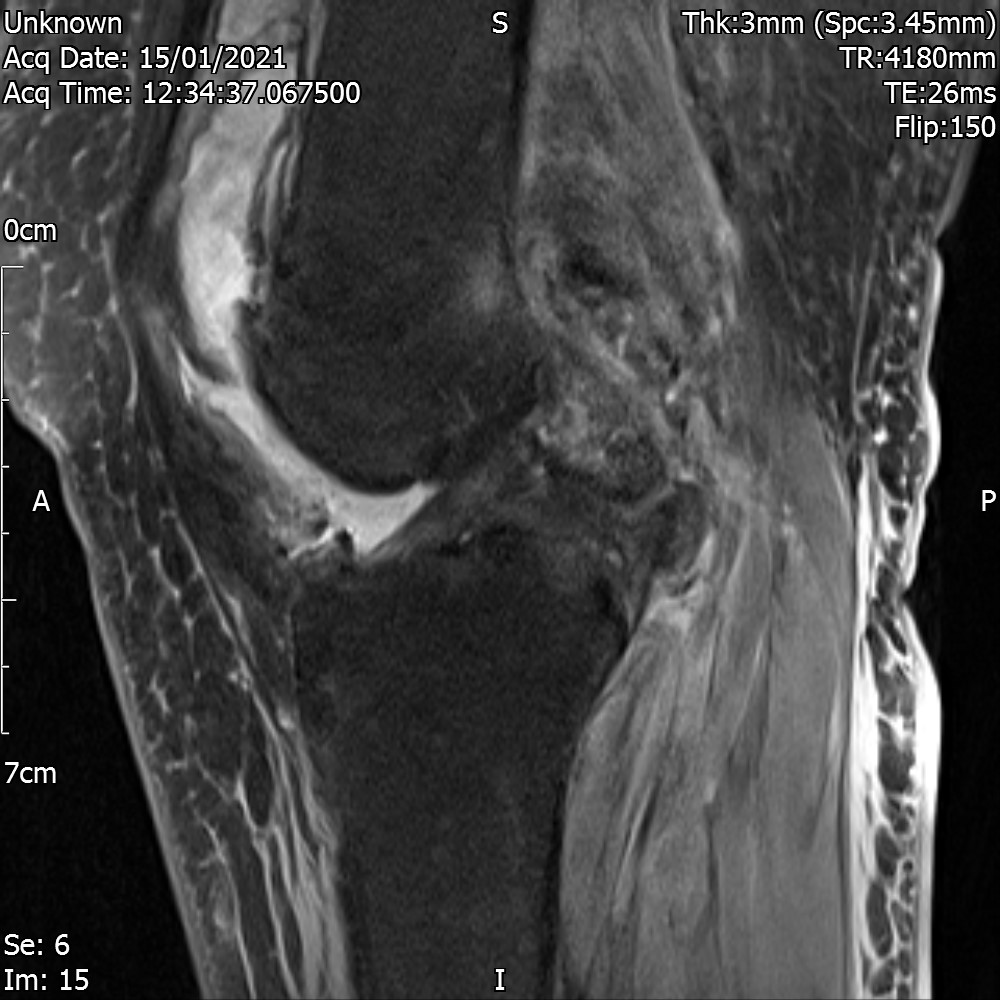
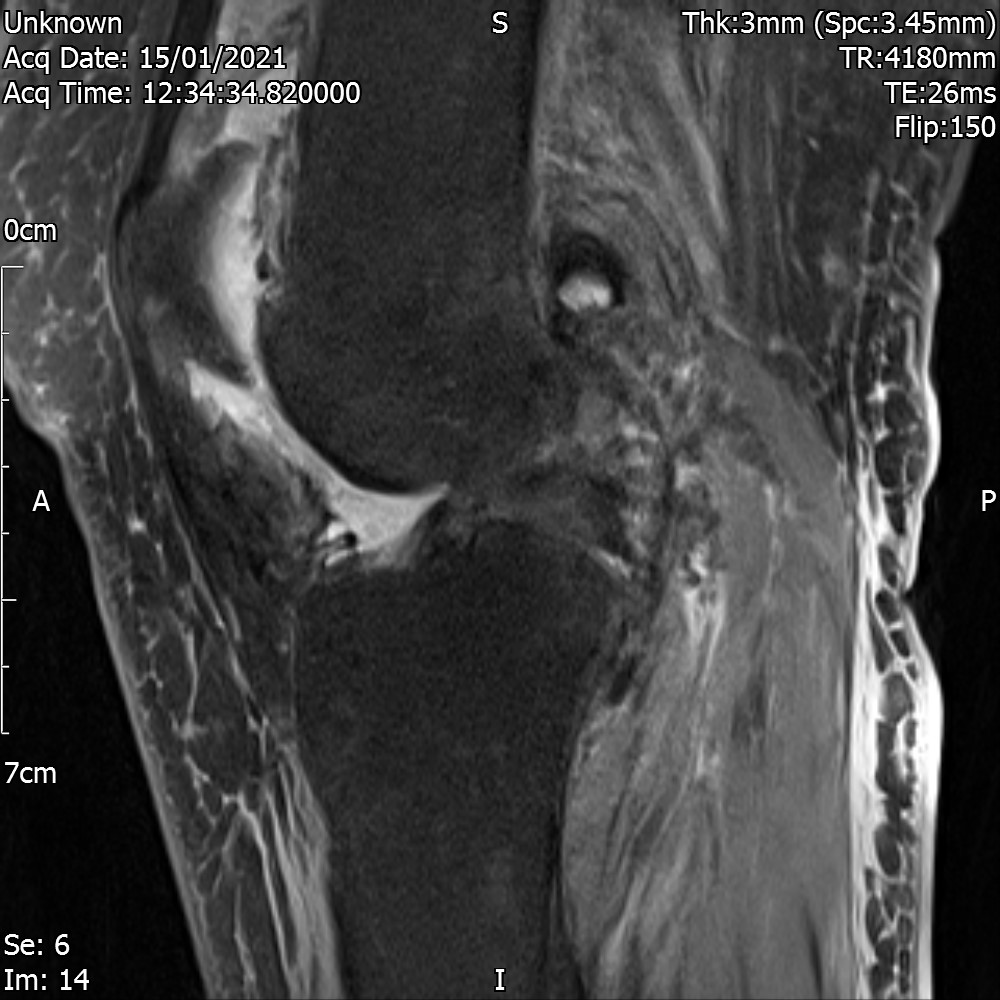
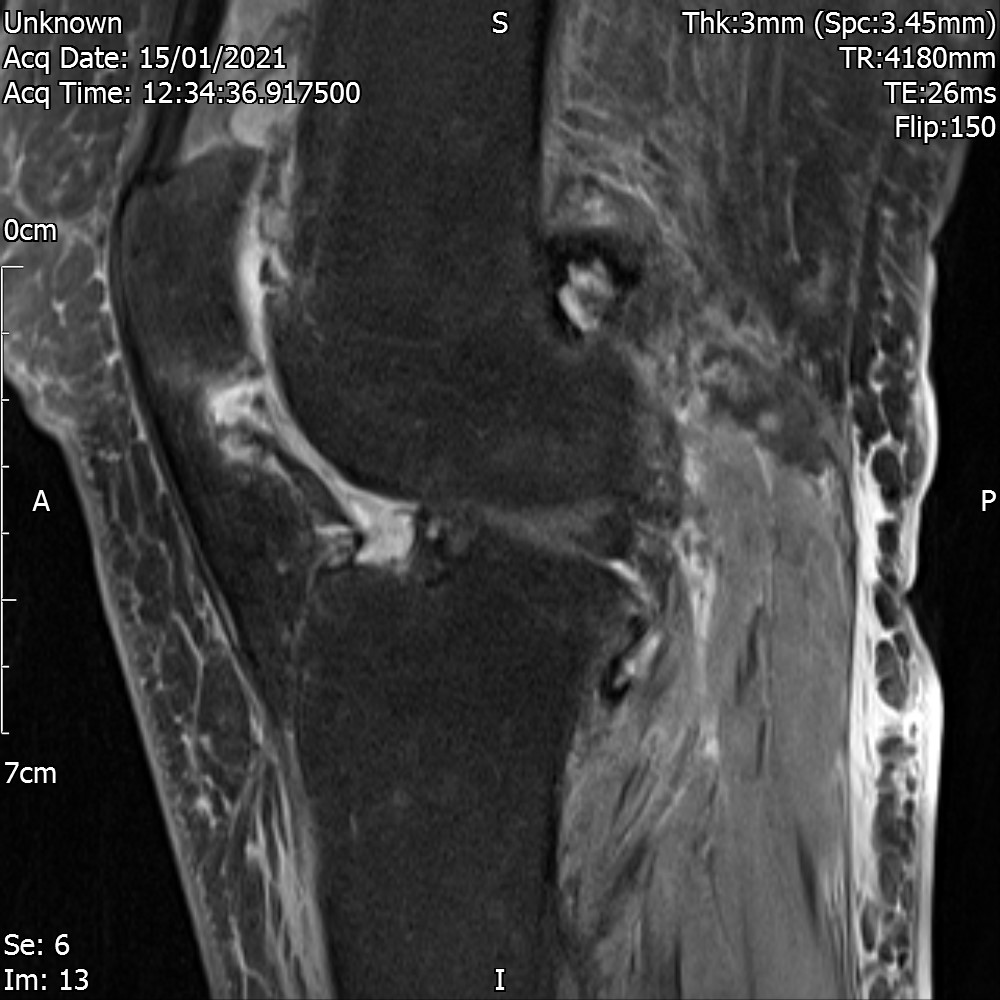
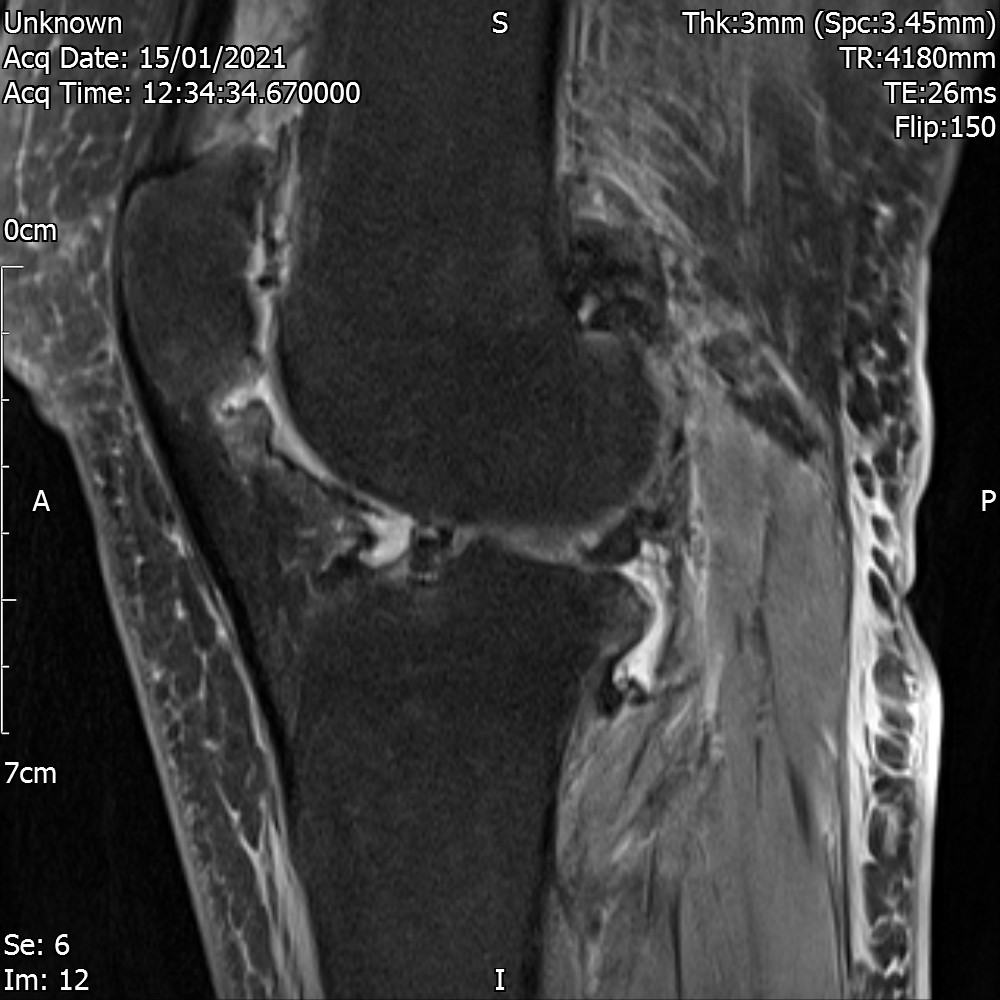
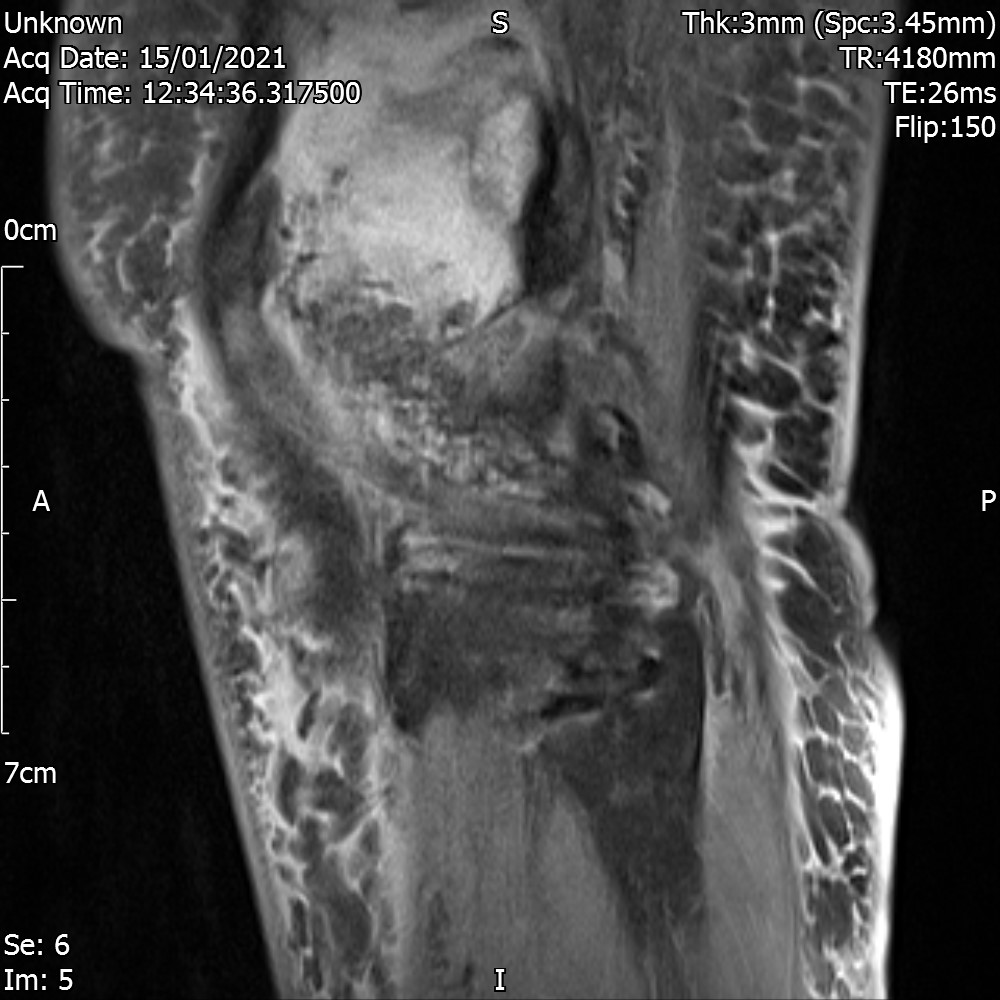
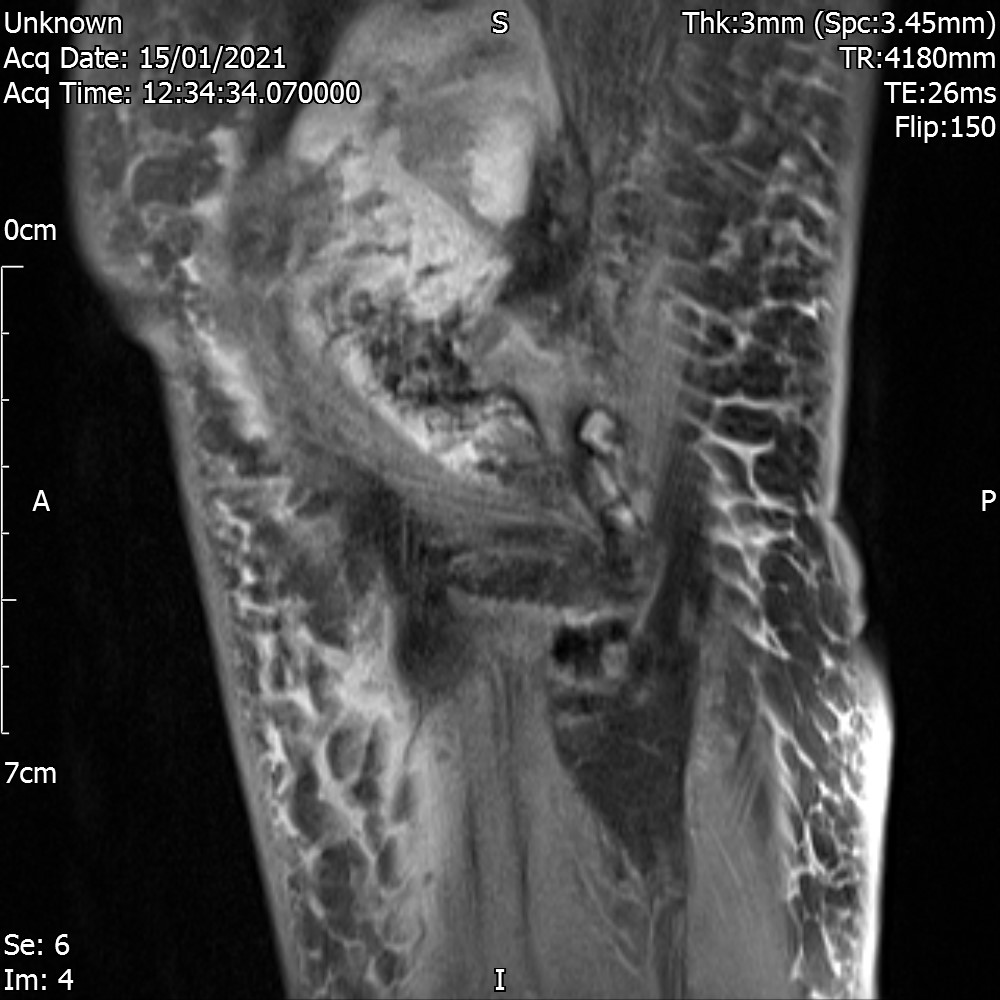
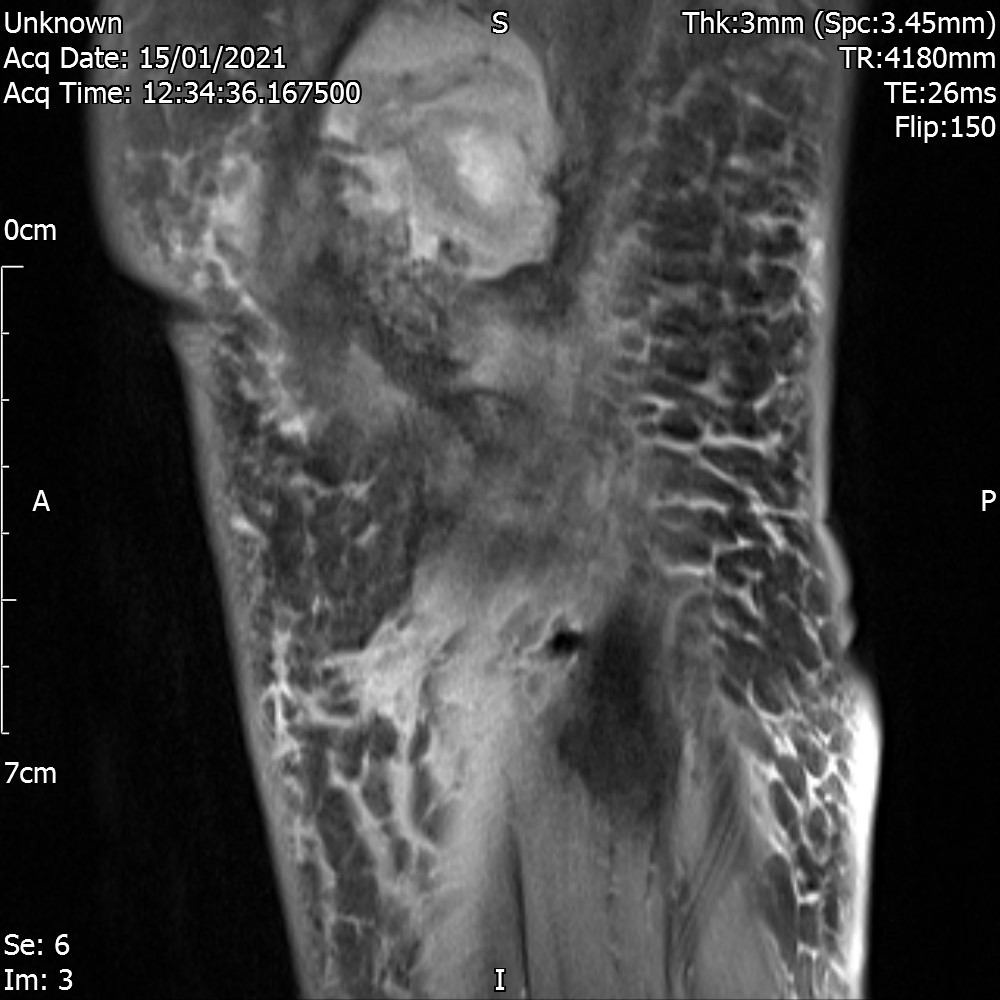
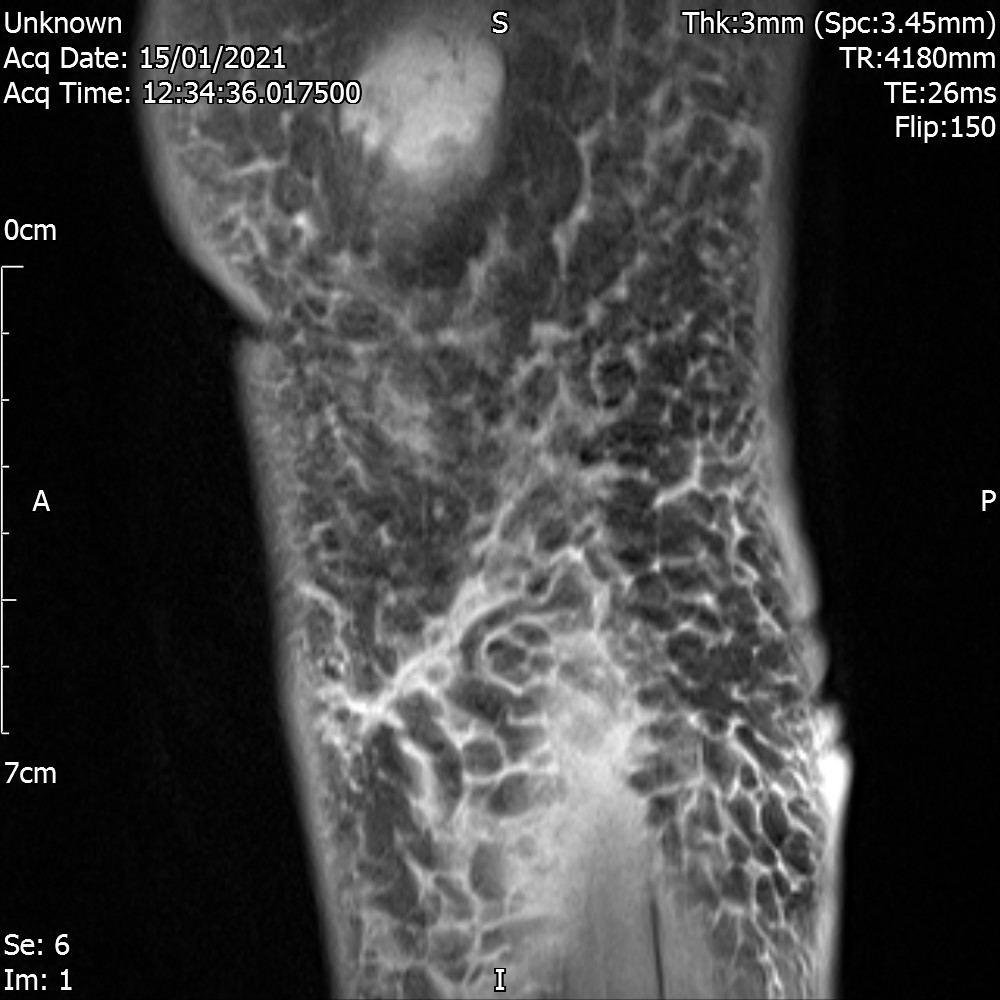
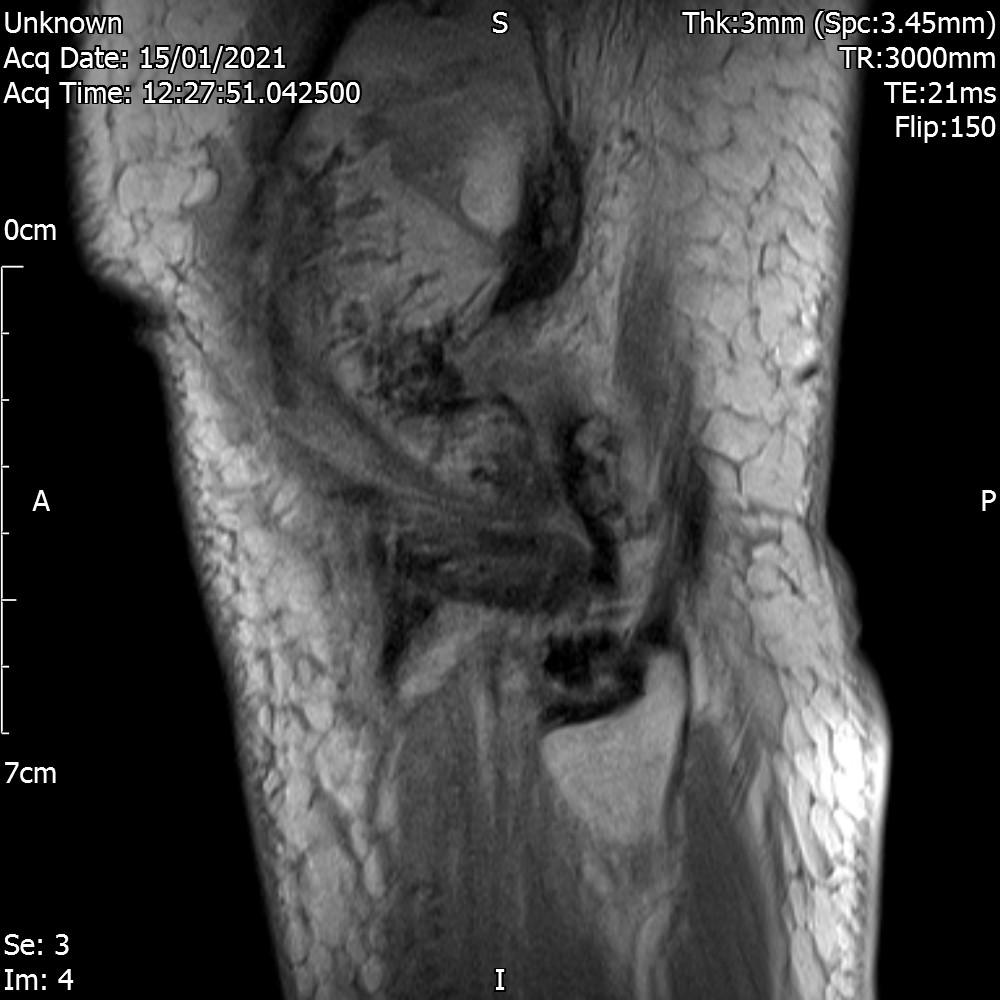
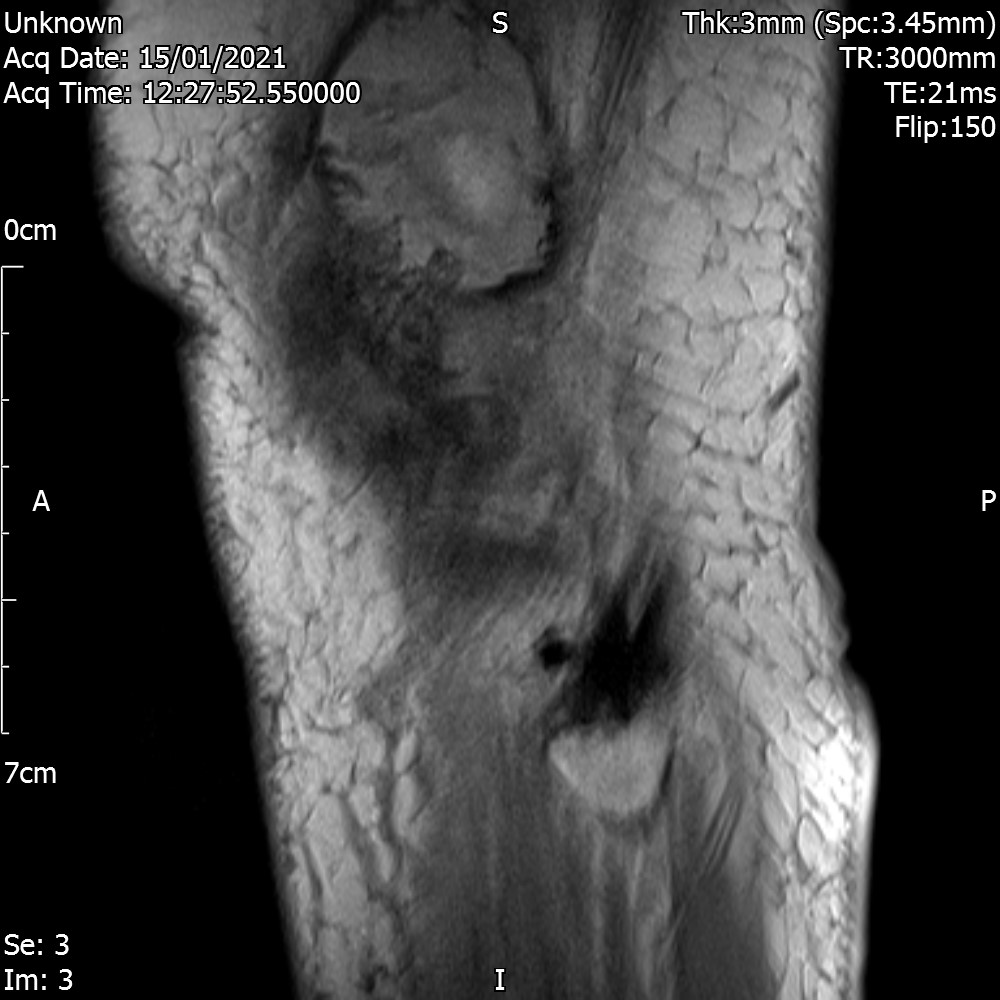
Saggital View – FS
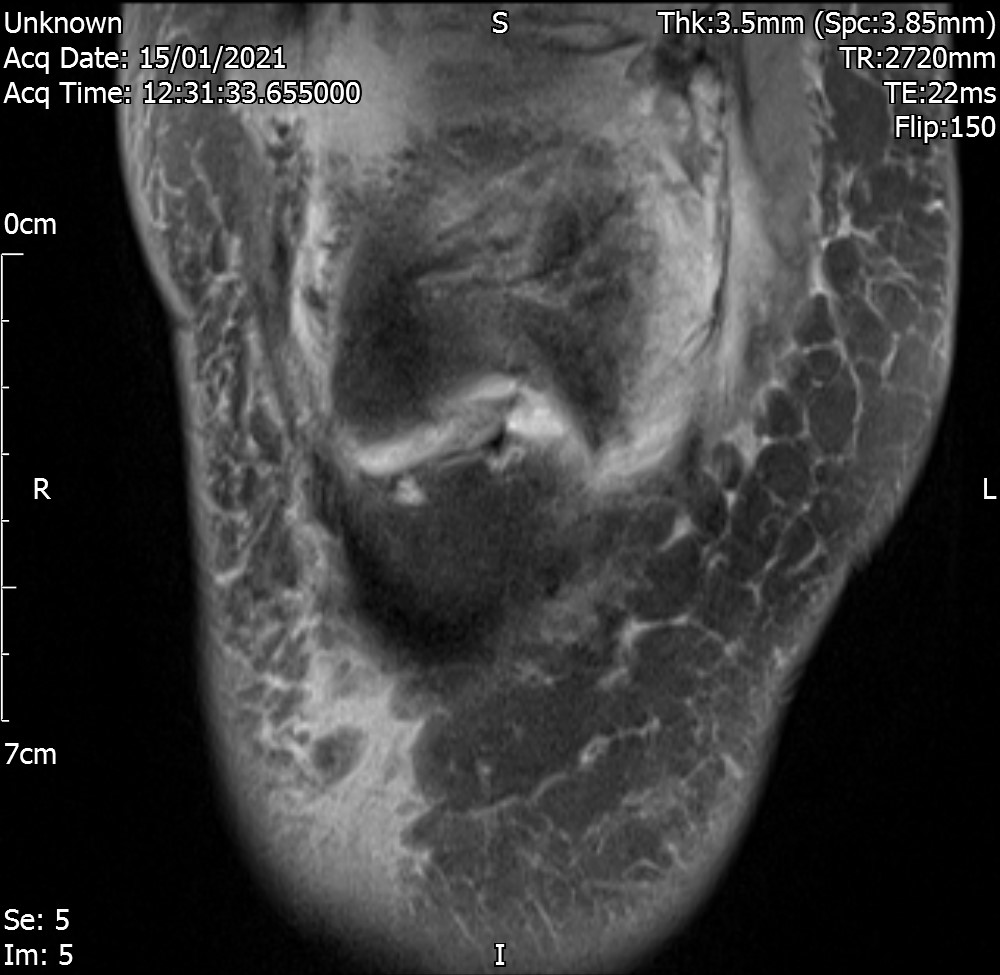
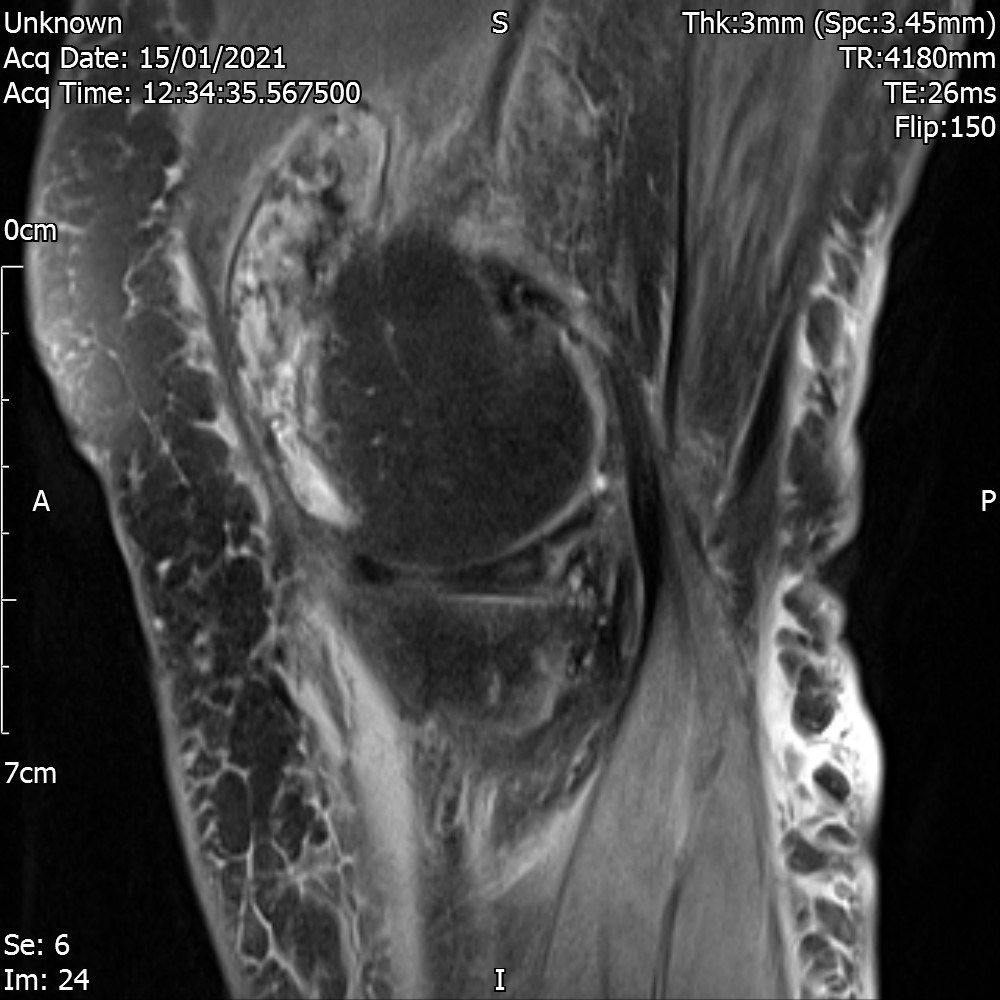
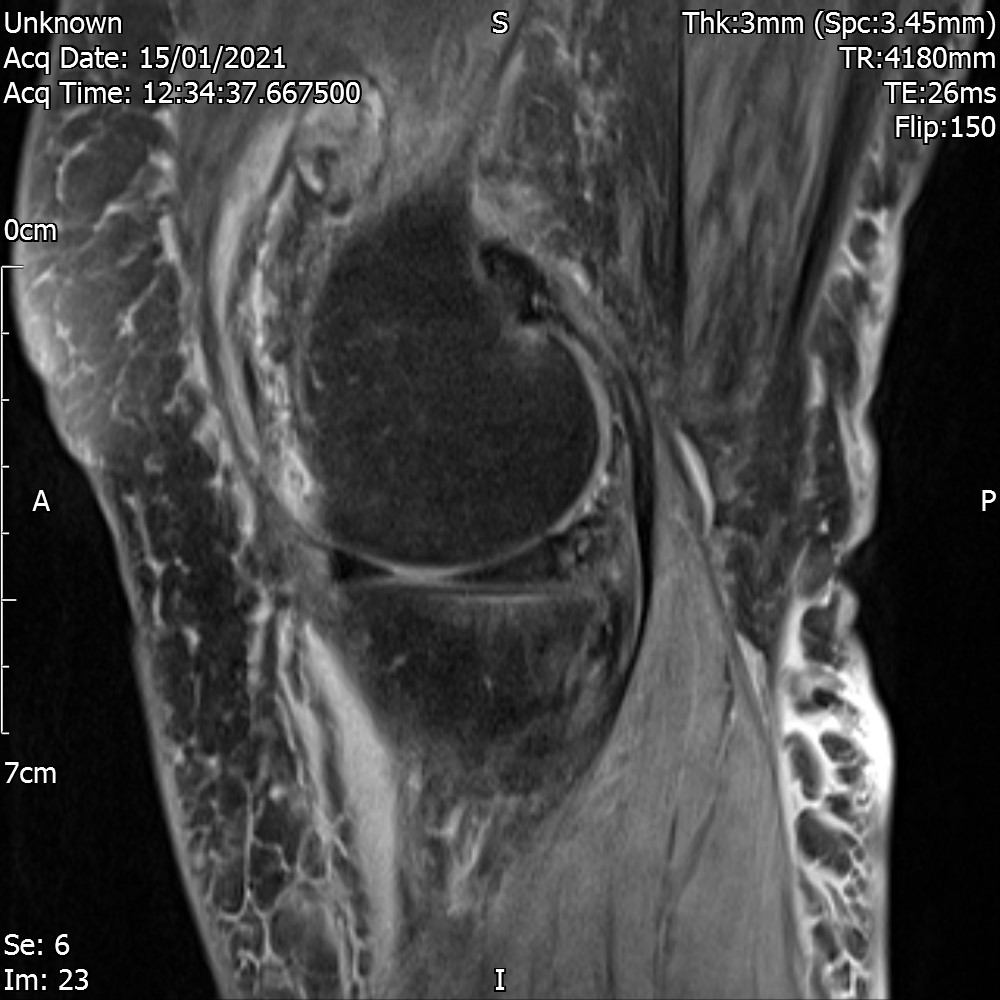
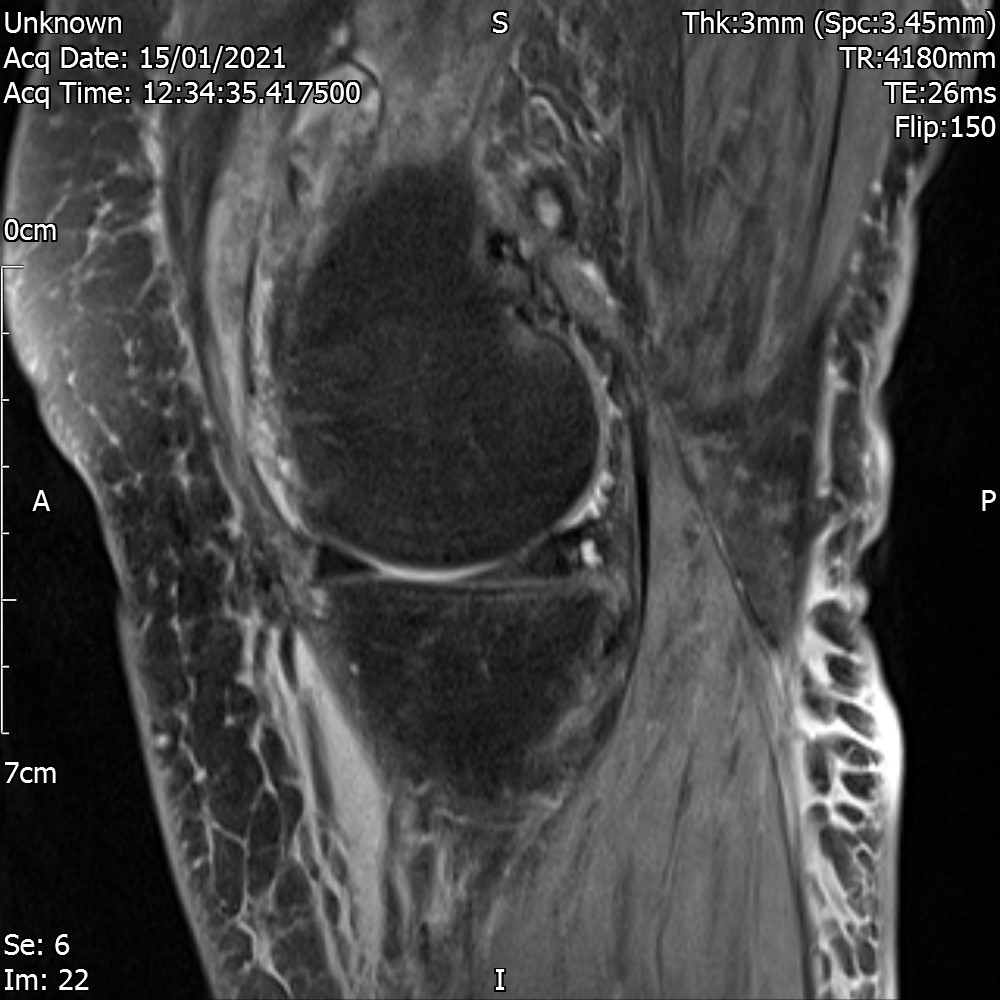
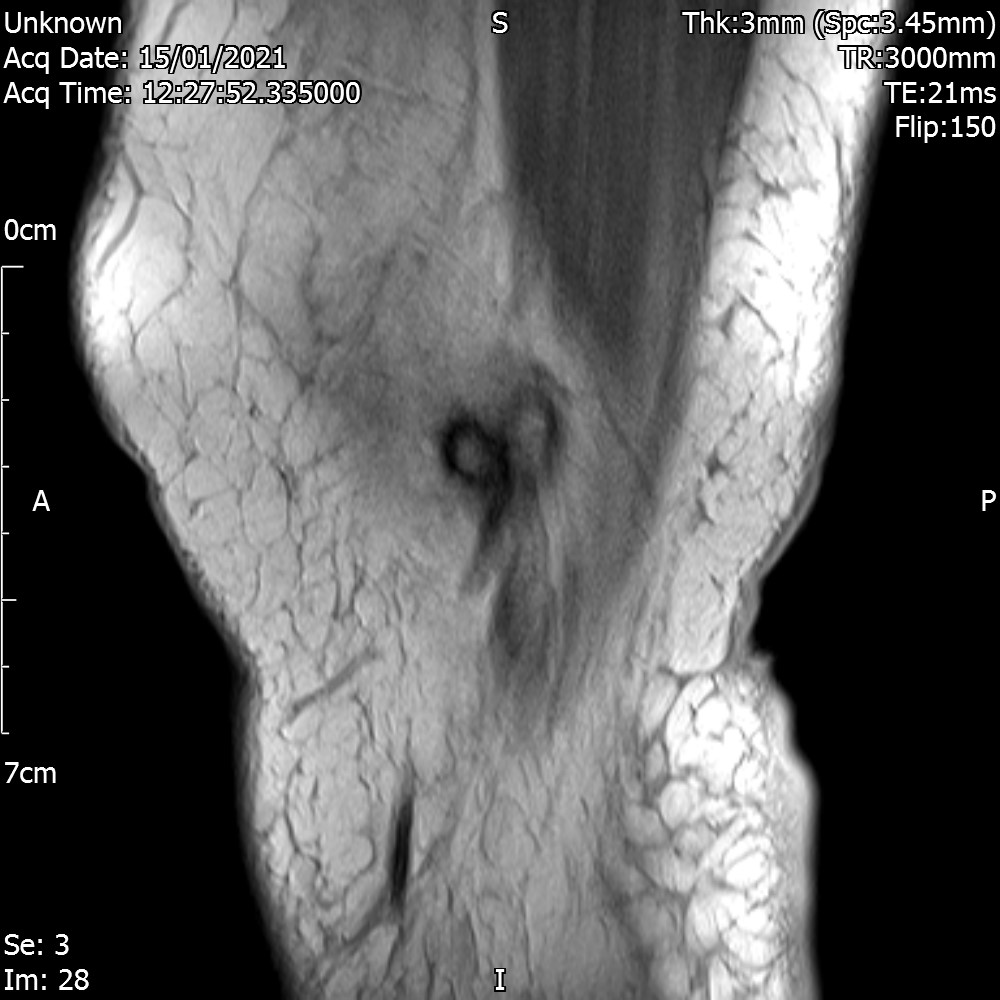
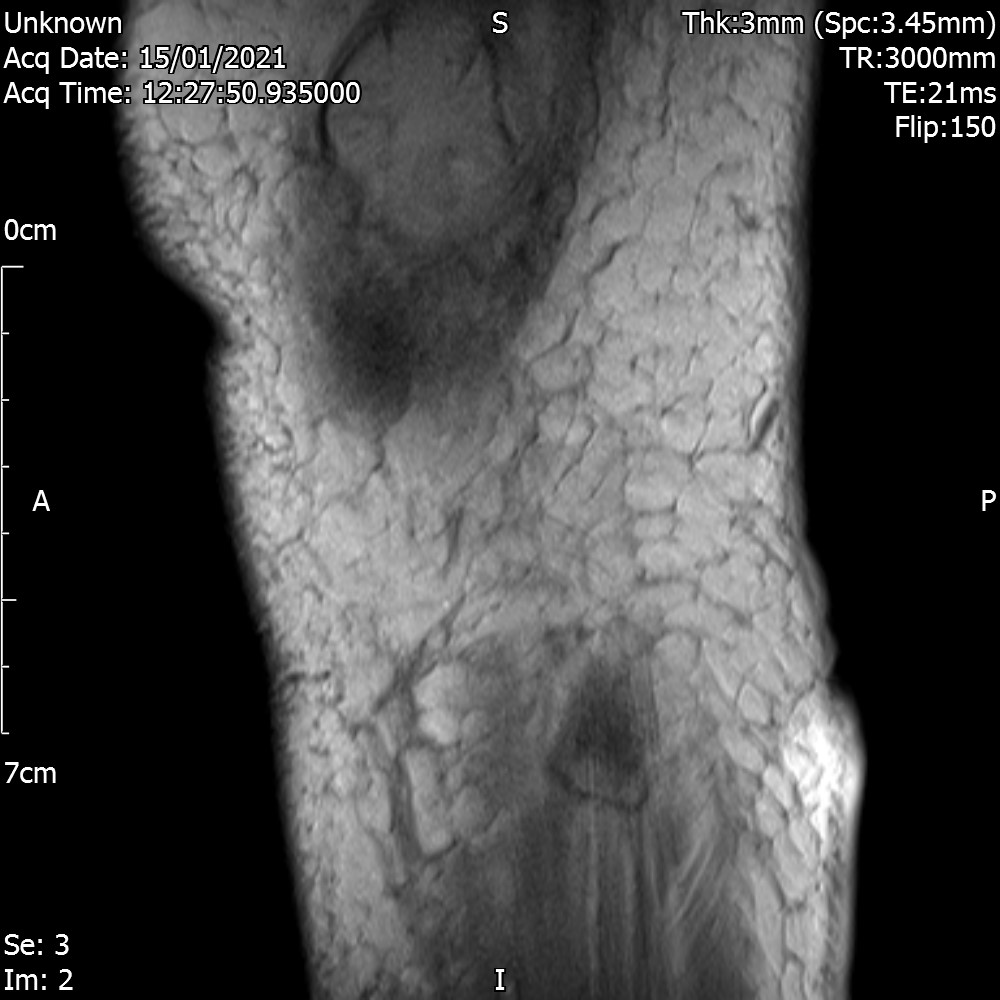
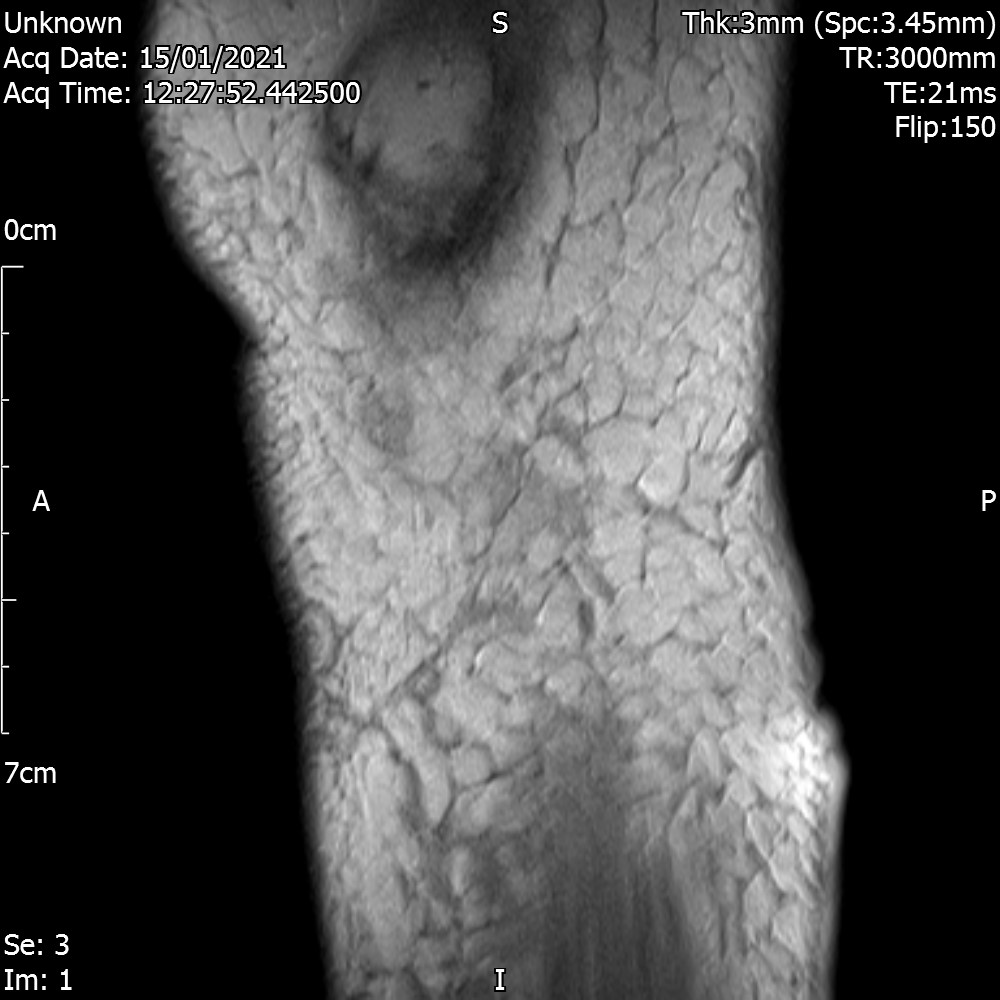
Saggital View – TSE
There is a horizontal tear through the posterior horn of the medial meniscus. There is also an extensive tear through the lateral meniscus.
The anterior and posterior cruciate ligaments are intact.
There is fluid outside the medial collateral ligament indicating a sprain. The lateral collateral ligament appears intact.
The quadriceps and patellar tendons appear normal.
Moderate joint effusion with evidence of synovitis and synovial thickening with some susceptibility artefact suggestive of PVNS. There are multiple loose bodies. There is moderate loss of the retropatellar cartilage particularly overlying the medial facet. There is early to moderate lateral tibiofemoral and medial tibiofemoral osteoarthritis.
CONCLUSION
Horizontal tear through the posterior horn of the medial meniscus and an extensive tear through the lateral meniscus. Tricompartmental osteoarthritis. Synovitis with evidence of PVNS.
Loose bodies. Consider a repeat MRI scan with IV gadolinium to exclude any evidence of synovial sarcoma.
Outcome
The patient was referred to the Sarcoma unit who concluded the following.
- We reviewed the imaging on the patient. There is no evidence of a malignancy on reviewing the knee MRI scan. We suspect she has had a haemarthrosis as a result of being on Apixaban. All the appearances are suggestive of a cirrhotic synovitis in the knee. We do not consider that she needs to be seen in the Sarcoma Clinic as such. If she continues to have pain, she may well be better to be referred to either the Rheumatologist or the Acute Knee Clinic. We are happy to take her off the two-week pathway. There is no evidence of a suspected sarcoma.
Patient reported that the knee was better and wanted to give it more time to settle. There was no further referral.