Intestinal Tumour
Published on Apr 6, 2022
38 male
History of low back pain - approx 5 years.
Feb 2021 - attended GP surgery for back pain + left leg pain. Gave a 2 month history for symptoms. Jumped out of a van which made the symptoms worse. Also reported P+N in the left leg. No B+B issues. Booked for FCP appt next day. Patient DNA.
July 2021 - attended A&E for GI, Abdominal pain. Urine test - NAD. Diagnosed with sciatica.
Aug 2021 - reported to GP for back and leg pain. Prescribed pain meds by GP. Referred to MSK service.
Sep 2021 - seen in physiotherapy. As patient reported being systemically unwell, had reported 1 episode of vomiting and night sweats, the patient was asked to visit A&E after a discussion with Ortho oncall.
Sep 2021 (same day) - attended A&E for back pain. Was sent by physiotherapist as the patient complained of 1 episode of vomiting and 3 days of night sweats. Exam ruled out any cauda equina. Diagnosed with chronic back pain and sciatica. Advised to continue with physio.
Sep 2021 - patient reported to GP with 2 week history of nausea and vomiting. ? Norovirus. Given prochlorperazine.
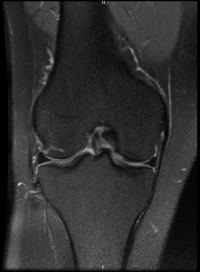
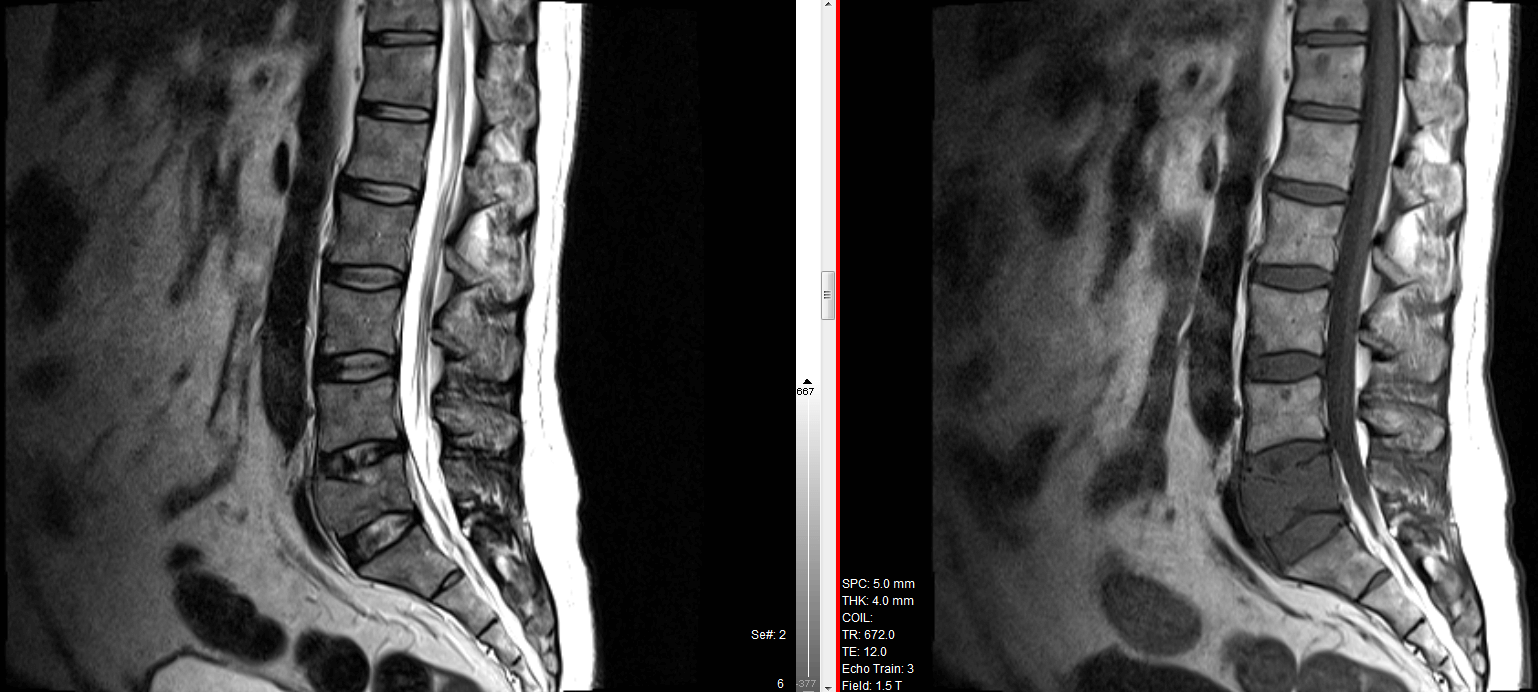
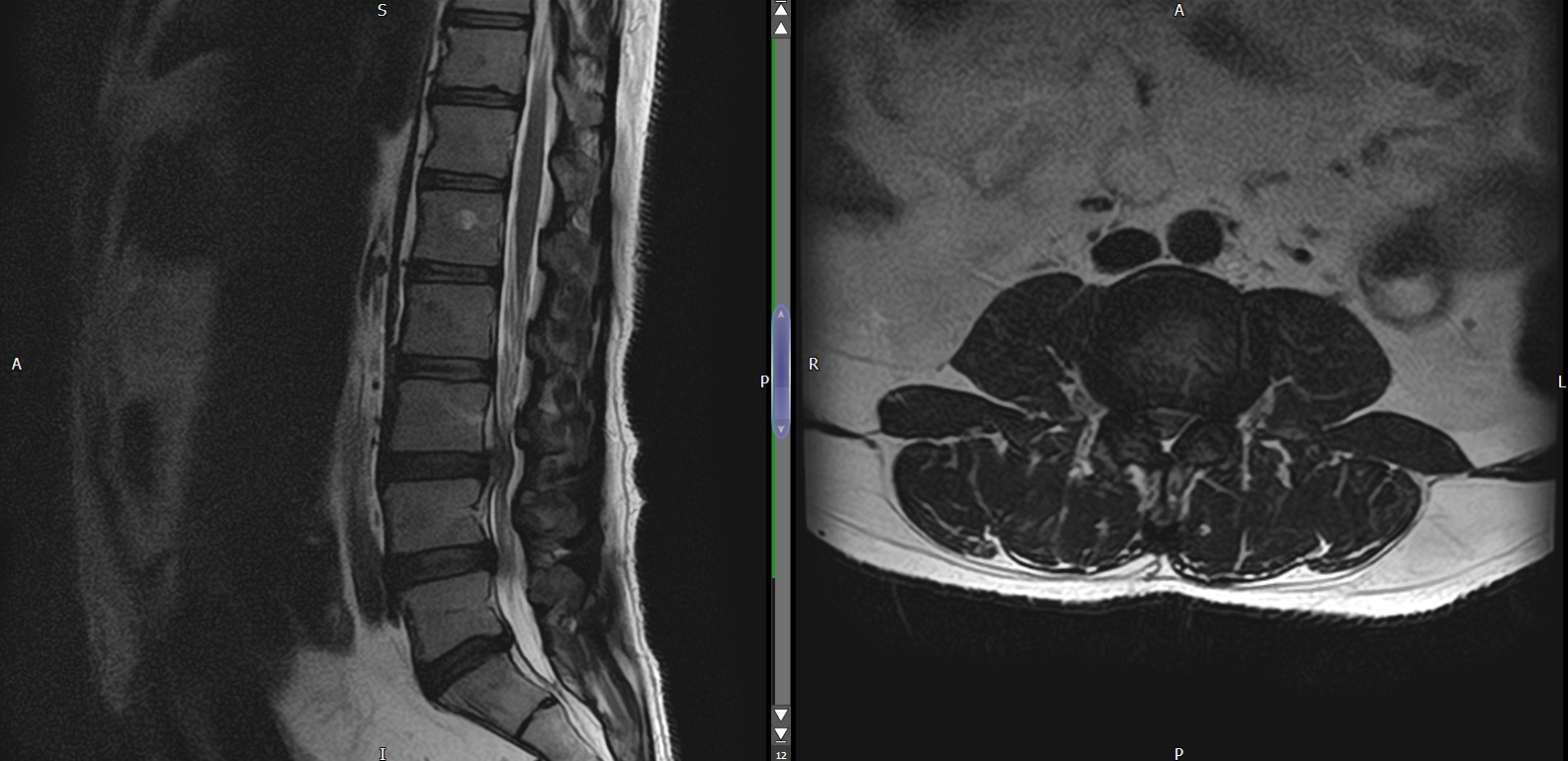
October 2021 - sent for MRI scan by physio for lumbar spine.
October 2021 - MRI arranged by physio showed a very large disc at L5/S1. Referred urgently to Spinal Ortho.
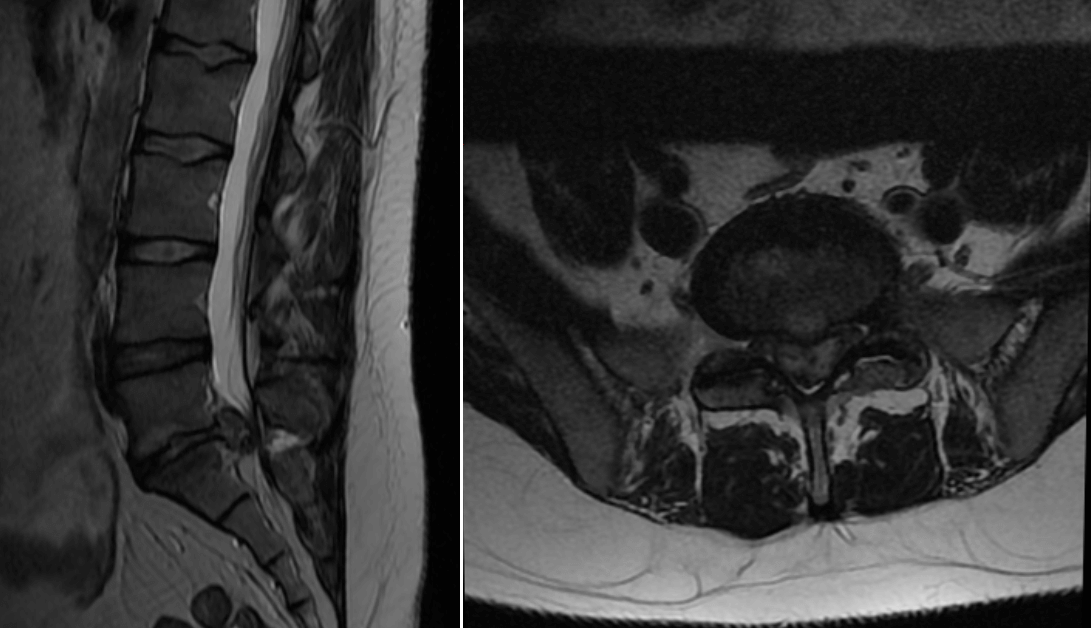
October 2021 - seen in spinal ortho. Planned urgent surgery.
Nov 2021 - underwent L5/S1 discectomy.
- Pre-op bloods showed CRP of 90, ALT 53, Bilirubin and ALP normal. Patient advised to see GP.
Nov 2021 (late) - patient sees GP re above. GP requests LFT and U&E.
Dec 2021 (early) - patient attends A&E for shortness of breath and right sided chest pain. Sent home with codeine.
Same day - patient see GP for dyspnoea. GP suspects VTE or PE. Refers back to AECU (Ambulatory Emergency Care Unit) to exclude PE.
Next day - Patient visits hospital. Blood test shows raised D dimer, raised LFT. Patient undergoes a CT PA (CT Pulmonary Angiogram) for suspected PE. CT negative for PE.
- D Dimer: 12020 ug/L (0 - 500)
- CRP: 169 (0 - 5)
- ALP: 202 (40 - 150)
- ALT: 72 (10 - 35)
Physician concludes - "pain and raised blood work due to recent operation and need for greater analgesia". Patient is admitted.
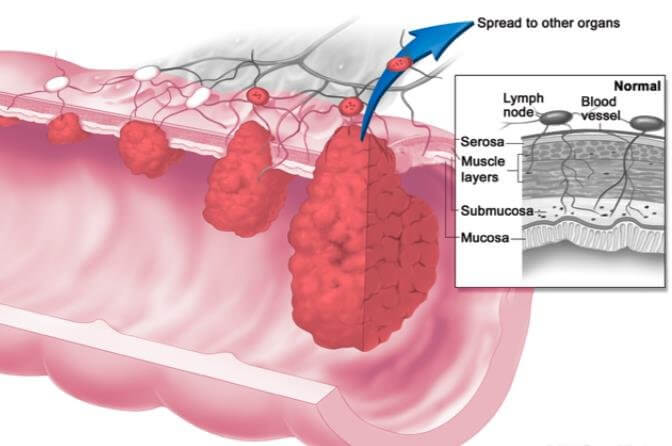
Next day - Patient undergoes CT Abdomen, Pelvis with contrast. Shows extensive hepatic metastatic disease with no definite primary in chest, abdomen and pelvis. Liver biospy for tissue diagnosis is suggested.
3 days later patient is given a call by consultant for procedure for biopsy but patient reported fever, nausea, vomiting and RUQ pain. Patient was brought in and admitted for IV antibiotics for suspected infection. Treated for 8 days with IV antibiotics.
- Liver biopsy revealed metastatic adenocarcinoma of lower GI origin.
- Imaging revealed transverse colon tumour with extensive mets.
Referred to oncology. Oncologist history review further mentioned that the patient had weight loss with waistline reducing by two sizes and also reduced appetite. Bowel movements were fine. Smoker, 25 cigarettes per day since the age of 17. MSH6 deficiency. Sister aged 45 died of bowel cancer. Treatment offered was chemotherapy. Also suggested to have genetic consultation for children to rule out genetic deficiencies.