Courtesy of Neil Langridge (Consultant Physiotherapist)
Key questions to exclude CES
Physiotherapist: So you have had some increased frequency of bladder function…
Patient: Yes…
Physiotherapist: Have you noticed any other change in bladder or bowel function?
Patient: No just that I seem to be passing urine a lot more frequently…
Physiotherapist: Ok. I would like to know a little bit more about how your bladder is behaving if that is ok? I am going to ask you some other important questions that may seem unrelated to your back pain…
Question 1: What questions might you ask at this point?
Model answer: Now that the patient has been focused on important questions, you should explain CES using the clinical cue card and give the patient the CES credit card and go through each question.
Physiotherapist: Ok that’s very reassuring, so the only thing that has changed is that you are passing urine a lot more frequently…
Patient: Yes…
Physiotherapist: Have you ever experienced this before?
Patient: No not really…
Physiotherapist: I see you are on a few medications to help pain and one to help leg pain, pregabalin?
Patient: Yes…
Physiotherapist: Did your change in bladder function begin before or after the medication began?
Patient: Oh after definitely because I wondered if it was because I was taking more water to swallow my tablets.
Thoughts: In this scenario the person describes just one risk factor of CES but no other worrying symptoms were extracted from a detailed subjective history and the person is getting better. The altered frequency could be caused by the medication (or pain). This lady is still worthy of safety netting regarding CES but CES is unlikely.
Key questions to exclude spinal infection
Physiotherapist: Do you feel fit and well in yourself?
Patient: Yes…
Physiotherapist: Have you noticed a fever or raised temperature particularly when the back pain started?
Patient: No…
Physiotherapist: You were in Africa for 10 years, whereabouts?
Patient: Somalia…
Question 2: What should you ask at this point?
Model answer: As she has lived in Africa, where tuberculosis (TB) is endemic, you should check her Bacillus Calmette-Guérin (BCG) status.
Physiotherapist: Do you recall having a BCG injection?
Patient: Yes, I had an injection when I was at school and was rechecked when I went to live in Africa.
Physiotherapist: I note that you are a smoker, how many do you smoke a day?
Patient: I am more of a social smoker so maybe 2-3.
Physiotherapist: How long have you smoked for?
Patient: Oh since my 20s but on and off.
Physiotherapist: How confident do you feel about managing your diabetes, both day today, and in relation to your HbA1C?
Patient: Yes, it’s very stable and I am on the border.
Thoughts: In this scenario the person describes a number of risk factors for spinal infection, both smoking and diabetes have an effect on the immune system but in this case she describes a low level of smoking and she is confident managing her diabetes, both practically and clinically. She has lived in a country where TB is endemic but was immunised against TB. She is also living in London where there has been an increase in TB cases. She describes the leg pain as getting easier. Overall it is very unlikely that she has SI but should her back pain progressively worsen this might need to be re-evaluated.
Key questions to exclude malignancy
Physiotherapist: Can you tell me a little more about your breast cancer?
Patient: Yes of course. I was diagnosed 3 years ago, I can’t remember exactly what type it was but I was treated successfully.
Question 3: What should you ask about at this point?
Model answer: You should seek more details of the treatment she received for her breast cancer.
Physiotherapist: What treatment did you have?
Patient: I had to have a lump removed and then radiotherapy afterwards.
Physiotherapist: That must have been quite tough. Do you remember if you had any lymph nodes removed?
Patient: No, not that I can remember.
Physiotherapist: You’ve told me that you have had episodes of back pain in the past, does this feel like one of those episodes?
Patient: Yes it does feel similar, I have had this before in my back but never in my leg, but I think my leg feels better than when it first started.
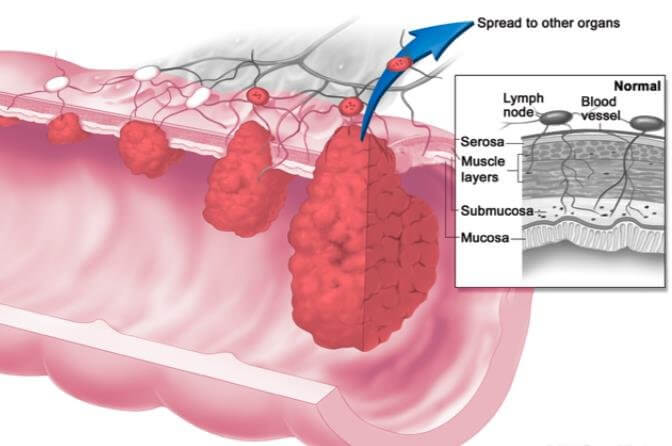
Thoughts: The person describes cancer that could metastasise but she is not being woken at night and the back pain is familiar, although it’s the first episode of leg pain. There are no other red flags and at this time but it would be important to monitor any change in the patient’s symptoms over time.
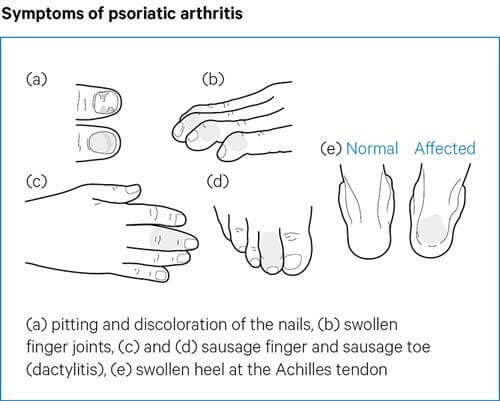
Key questions to exclude spondyloarthritis
Physiotherapist: You mentioned that you feel stiff in the morning which can last for an hour…
Patient: Yes that’s right, it takes me a while to get going then I’m alright.
Physiotherapist: Have you noticed this before now, when you have had previous episodes of back pain?
Patient: Not that I can remember.
Question 4: What should you ask about the timing of the pain?
Model answer: You should check if the pain is worse when she is resting, or better when she is active, as this would be a strong indicator for further investigation.
Physiotherapist: Is your back pain aggravated by rest or is it better with activity?
Patient: Not really, it depends on what I am doing. If I walk too much it’s uncomfortable but if I sit too much its also uncomfortable.
Physiotherapist: So, sometimes back pain can be caused by inflammatory conditions and so I want to ask you some specific questions which will help me to decide whether this is the case. Is that ok?
Patient: Yes of course that’s fine.
Physiotherapist: Have you had any pain or noticed any swelling in any of your joints, or have you experienced any tendon issues?
Patient: I sprained my ankle a couple of years ago.
Physiotherapist: Ok so you sprained your ankle a while ago. Is there any family history of arthritis?
Patient: My mother has arthritis, she had to have a hip replacement last year.
Physiotherapist: Has she recovered well from the hip replacement?
Patient: Yes it was very good, she has discovered her independence again.
Physiotherapist: That’s good to hear. Can you tell me if your sleeping pattern has changed since this episode?
Patient: It was waking me up when it first started but not so much now.
Question 5: What should you ask about at this point?
Model answer: You should check if the pain is worse in the second half of the night, as this would be a strong indicator for further investigation.
Physiotherapist: Was it waking you up at a specific time in the night?
Patient: No, more when I turned over.
Physiotherapist: Ok, can you tell me if you suffer from any skin conditions?
Patient: No…
Physiotherapist: Any problems with your digestive system?
Patient: No…
Physiotherapist: That’s good, have you noticed any problems with your eyes such as swelling and redness?
Patient: No.
Thoughts: The person describes back pain which is episodic rather than chronic in nature. Whilst she describes being stiff in the morning for an hour this seems to be improving and she is not woken in the early hours. She doesn’t complain of any extra-articular features associated with SpA.
Key questions to exclude spinal fracture
Physiotherapist: Have you had any broken bones in the past?
Patient: Yes – I had a wrist fracture after a fall 3 years ago.
Physiotherapist: Tell me about the fall.
Patient: I tripped in the street and fell onto my outstretched hand.
Question 6: What should you ask about in relation to broken bones?
Model answer: You should check if there is any family history of osteoporosis and early menopause.
Physiotherapist: Ok thanks. Is there a history of osteoporosis or thin bones in your family?
Patient: Yes my mum had osteoporosis.
Physiotherapist: There are some things that affect your bone strength, so I am going to ask you some further questions that relate to these. Have you been through the menopause – if so how old were you?
Patient: Yes, I was 42.
Physiotherapist: Sometimes having an early menopause can cause thinning of your bones but this is just one factor. Did your mother or any other female relatives have an early menopause?
Patient: Yes my mum and sister, both at 43.
Physiotherapist: Ok, are you a smoker? If so, how long have you smoked for?
Patient: Oh, since my 20s but on and off – only 2 or 3 a day.
Physiotherapist: What about alcohol – how much do you drink per week?
Patient: Oh, about 2 bottles of wine a week I think – have done for years.
Physiotherapist: Have you had your vitamin D level checked?
Patient: Yes it was fine.
Physiotherapist: OK- what about steroid tablets – have you ever had to use these?
Patient: I did have some a few years ago for polymyalgia – I took them for about 2 years.
Physiotherapist: Do you know what dose you took?
Patient: I think I started on 30 mg and eventually came down to 1 and then stopped.
Physiotherapist: Ok, what about your diet – do you consider you have a healthy diet?
Patient: Just the normal meat and two veg.
Physiotherapist: And finally, do you have any gut problems, like Crohn’s disease or other dietary issues?
Patient: No, nothing like that.
Thoughts: In this scenario, the patient describes several risk factors for osteoporosis, including an early menopause, her alcohol intake which is above recommended levels and has been for a long time. She has also had a previous fracture and has a history of prolonged and high level steroid use, all of which put her at risk of osteoporosis and potential fracture.