NSAIDs
Paracetamol - Adult - 0.5–1 g every 4–6 hours; maximum 4 g per day.
- Pregnancy - Not known to be harmful.
- Breast feeding - Amount too small to be harmful.
- Hepatic & Renal impairment - exercise caution.
- Paracetamol is similar in efficacy to aspirin, but has no demonstrable anti-inflammatory activity; it is less irritant to the stomach and for that reason is now generally preferred to aspirin, particularly in the elderly. Overdosage with paracetamol is particularly dangerous as it may cause hepatic damage which is sometimes not apparent for 4 to 6 days.
Ibuprofen - Adult - usual dose 400mg TDS
- Ibuprofen gel 5% - Apply up to 3 times a day. (Treatment in knee or hand OA)
- Fenbid Forte - Apply up to 4 times a day, therapy should be reviewed after 14 days.
- Contraindications - GI bleed, active GI ulceration, history of GI bleeding related to NSAID use, history of recurrent GI ulceration (two or more distinct episodes), severe heart failure, varicella infection.
- Contraindicated in patients with a history of hypersensitivity to aspirin or any other NSAID—which includes those in whom attacks of asthma, angioedema, urticaria or rhinitis have been precipitated by aspirin or any other NSAID.
- Cautions - Allergic disorders; cardiac impairment (NSAIDs may impair renal function); cerebrovascular disease; coagulation defects; connective-tissue disorders; dehydration (risk of renal impairment); elderly (risk of serious side-effects and fatalities) (in adults); heart failure; history of gastro-intestinal disorders (e.g. ulcerative colitis, Crohn’s disease); ischaemic heart disease; may mask symptoms of infection; peripheral arterial disease; risk factors for cardiovascular events; uncontrolled hypertension.
- Fertility - long-term use of some NSAIDs is associated with reduced female fertility, which is reversible on stopping treatment.
- Pregnancy - avoid use. Avoid during the third trimester (risk of closure of fetal ductus arteriosus in utero and possibly persistent pulmonary hypertension of the newborn); onset of labour may be delayed and duration may be increased. Also avoid use of topical
- Breast feeding - Amount too small to be harmful but some manufacturers advise avoid.
- Hepatic & Renal impairment - Caution in mild to moderate impairment (increased risk of renal failure); avoid in severe impairment. Deterioration in renal function has also been reported after topical use.
Naproxen - Adult - MSK pain - 250mg BD or 500mg BD. Gout - Initially 750 mg, then 250 mg every 8 hours until attack has passed.
- Naproxen is one of the first choices because it combines good efficacy with a low incidence of side-effects (but more than ibuprofen).
- Contraindications and cautions similar to ibuprofen
Diclofenac - Adult - 75–150 mg daily in 2–3 divided doses.
- Voltarol SR 75mg - 1 tablet 1-2 times a day.
- Voltarol Emulgel - Apply 3–4 times a day, therapy should be reviewed after 14 days (or after 28 days for osteoarthritis).
- Contraindications and cautions similar to ibuprofen
Etodolac - Adult - 600 mg OD
- licensed for symptomatic relief of osteoarthritis and rheumatoid arthritis.
- etodolac is comparable in efficacy to naproxen.
Indometacin - Adult - 50–200 mg daily in divided doses.
- Indometacin MR (modified release) - 75 mg 1–2 times a day.
- Indometacin has an action equal to or superior to that of naproxen, but with a high incidence of side-effects including headache, dizziness, and gastro-intestinal disturbances.
Mefenamic Acid - Adult - 500mg TDS
- Indication - Pain and inflammation in rheumatoid arthritis and osteoarthritis.
- Mefenamic acid has minor anti-inflammatory properties. It has occasionally been associated with diarrhoea and haemolytic anaemia which require discontinuation of treatment.
Meloxicam - Adult - 7.5 mg once daily, then increased if necessary up to 15 mg once daily
- Meloxicam is licensed for the short-term relief of pain in osteoarthritis and for long-term treatment of rheumatoid arthritis and ankylosing spondylitis.
Nabumetone - Adult - 1 g OD, dose to be taken at night. Elderly - 0.5–1 g daily. For severe and persistent symptoms - 0.5–1 g, dose to be taken in the morning and 1 g, dose to be taken at night.
- Indication - Pain and inflammation in osteoarthritis and rheumatoid arthritis.
- Nabumetone is comparable in effect to naproxen.
Piroxicam - Adult - up to 20mg OD. Only initiated by a specialist.
- Piroxicam gel - Apply 3–4 times a day, 0.5% gel to be applied; review treatment after 4 weeks
- piroxicam should not be used as first-line treatment.
- in adults, use of piroxicam should be limited to the symptomatic relief of osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis.
- piroxicam should no longer be used for the treatment of acute painful and inflammatory conditions.
- concomitant administration of a gastro-protective agent should be considered.
- Piroxicam is as effective as naproxen and has a long duration of action which permits once-daily administration. However, it has more gastro-intestinal side-effects than most other NSAIDs, and is associated with more frequent serious skin reactions.
Sulindac - Adult - 200 mg BD for maximum duration 7–10 days in peri-articular disorders, dose may be reduced according to response; acute gout should respond within 7 days; maximum 400 mg per day.
- Sulindac is similar in tolerance to naproxen.
Tenoxicam - Adult 20mg OD. maximum duration of treatment 14 days.
- Tenoxicam is similar in activity and tolerance to naproxen. Its long duration of action allows once-daily administration.
Tolfenamic Acid - 200 mg, dose to be taken at onset, then 200 mg after 1–2 hours if required.
- Tolfenamic acid is licensed for the treatment of migraine.
Selective Cox-2 Inhibitors
Etoricoxib
- OA - Adult - 30 mg OD, increased if necessary to 60 mg OD.
- RA & AS - Adult - 60 mg OD, increased if necessary to 90 mg OD.
- Gout - 120 mg OD for maximum 8 days
Celecoxib - Adult - 100 mg BD, then increased if necessary to 200 mg BD, discontinue if no improvement after 2 weeks on maximum dose.
- Celecoxib and etoricoxib are licensed for the relief of pain in osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis; etoricoxib is also licensed for the relief of pain from acute gout.
Ketorolac trometamol and the selective inhibitor of cyclo-oxygenase-2, parecoxib, are licensed for the short-term management of postoperative pain.
- The selective inhibitors of COX-2, etoricoxib and celecoxib, are as effective as non-selective NSAIDs such as diclofenac sodium and naproxen.
- Although selective inhibitors can cause serious gastro-intestinal events, available evidence appears to indicate that the risk of serious upper gastro-intestinal events is lower with selective inhibitors compared to non-selective NSAIDs; this advantage may be lost in patients who require concomitant low-dose aspirin.
Aspirin has been used in high doses to treat rheumatoid arthritis, but other NSAIDs are now preferred.
Therapeutic effects
In single doses non-steroidal anti-inflammatory drugs (NSAIDs) have analgesic activity comparable to that of paracetamol, but paracetamol is preferred, particularly in the elderly.
In regular full dosage NSAIDs have both a lasting analgesic and an anti-inflammatory effect which makes them particularly useful for the treatment of continuous or regular pain associated with inflammation. Therefore, although paracetamol often gives adequate pain control in osteoarthritis, NSAIDs are more appropriate than paracetamol or the opioid analgesics in the inflammatory arthritides (e.g. rheumatoid arthritis) and in some cases of advanced osteoarthritis. NSAIDs can also be of benefit in the less well defined conditions of back pain and soft-tissue disorders.
Choice
Differences in anti-inflammatory activity between NSAIDs are small, but there is considerable variation in individual response and tolerance to these drugs. About 60% of patients will respond to any NSAID; of the others, those who do not respond to one may well respond to another. Pain relief starts soon after taking the first dose and a full analgesic effect should normally be obtained within a week, whereas an anti-inflammatory effect may not be achieved (or may not be clinically assessable) for up to 3 weeks. If appropriate responses are not obtained within these times, another NSAID should be tried.
NSAIDs reduce the production of prostaglandins by inhibiting the enzyme cyclo-oxygenase. They vary in their selectivity for inhibiting different types of cyclo-oxygenase; selective inhibition of cyclo-oxygenase-2 (COX-2) is associated with less gastro-intestinal intolerance. Several other factors also influence susceptibility to gastrointestinal effects, and a NSAID should be chosen on the basis of the incidence of gastro-intestinal and other side-effects.
Ibuprofen is a propionic acid derivative with anti-inflammatory, analgesic, and antipyretic properties. It has fewer side-effects than other non-selective NSAIDs but its anti-inflammatory properties are weaker. It is unsuitable for conditions where inflammation is prominent. Dexibuprofen is the active enantiomer of ibuprofen. It has similar properties to ibuprofen and is licensed for the relief of mild to moderate pain and inflammation.
Other propionic acid derivatives:
Flurbiprofen may be slightly more effective than naproxen, and is associated with slightly more gastro-intestinal side-effects than ibuprofen.
Ketoprofen has anti-inflammatory properties similar to ibuprofen and has more side-effects. Dexketoprofen, an isomer of ketoprofen, has been introduced for the short-term relief of mild to moderate pain.
Tiaprofenic acid is as effective as naproxen; it has more side-effects than ibuprofen.
Drugs with properties similar to those of propionic acid derivatives:
Phenylbutazone is licensed for ankylosing spondylitis, but is not recommended because it is associated with serious side-effects, in particular haematological reactions; it should be used only by a specialist in severe cases where other treatments have been found unsuitable.
Dental and orofacial pain
Most mild to moderate dental pain and inflammation is effectively relieved by NSAIDs. Those used for dental pain include ibuprofen, diclofenac sodium, and diclofenac potassium.
Considerations in the elderly
The use of NSAIDs in elderly patients is potentially inappropriate (STOPP criteria) if prescribed:
- with a vitamin K antagonist, direct thrombin inhibitor or factor Xa inhibitor in combination (risk of major gastrointestinal bleeding);
- with concurrent antiplatelet agent(s) without proton pump inhibitor (PPI) prophylaxis (increased risk of peptic ulcer disease);
- in a history of peptic ulcer disease or gastrointestinal bleeding, unless with concurrent PPI or H2-receptor antagonist (risk of peptic ulcer relapse)—not including COX-2 selective NSAIDs;
- with concurrent corticosteroids without PPI prophylaxis (increased risk of peptic ulcer disease);
- in patients with an eGFR less than 50 mL/minute/1.73 m2 (risk of deterioration in renal function);
- in severe hypertension or severe heart failure (risk of exacerbation);
- for long-term (longer than 3 months) symptom relief of osteoarthritis pain where paracetamol has not been tried (simple analgesics are preferable and usually as effective for pain relief);
- for chronic treatment of gout where there is no contraindication to a xanthine-oxidase inhibitor (xanthine-oxidase inhibitors are first choice prophylactic drugs in gout);
- a COX-2 selective NSAID in concurrent cardiovascular disease (increased risk of myocardial infarction and stroke).
Asthma
Any degree of worsening of asthma may be related to the ingestion of NSAIDs, either prescribed or (in the case of ibuprofen and others) purchased over the counter.
NSAIDs and cardiovascular events
All NSAID use (including COX-2 selective inhibitors) can, to varying degrees, be associated with a small increased risk of thrombotic events (e.g. myocardial infarction and stroke) independent of baseline cardiovascular risk factors or duration of NSAID use; however, the greatest risk may be in those receiving high doses long term.
COX-2 selective inhibitors, diclofenac (150 mg daily) and ibuprofen (2.4 g daily) are associated with an increased risk of thrombotic events. Although there are limited data regarding the thrombotic effects of aceclofenac, treatment advice has been updated in line with diclofenac, based on aceclofenac's structural similarity to diclofenac and its metabolism to diclofenac. The increased risk for diclofenac is similar to that of licensed doses of etoricoxib. Naproxen (1 g daily) is associated with a lower thrombotic risk, and low doses of ibuprofen (1.2 g daily or less) have not been associated with an increased risk of myocardial infarction.
The lowest effective dose of NSAID should be prescribed for the shortest period of time to control symptoms and the need for long-term treatment should be reviewed periodically.
NSAIDs and gastro-intestinal events
All NSAIDs are associated with serious gastro-intestinal toxicity; the risk is higher in the elderly. Evidence on the relative safety of non-selective NSAIDs indicates differences in the risks of serious upper gastro-intestinal side-effects—piroxicam, ketoprofen, and ketorolac trometamol are associated with the highest risk; indometacin, diclofenac, and naproxen are associated with intermediate risk, and ibuprofen with the lowest risk (although high doses of ibuprofen have been associated with intermediate risk). Selective inhibitors of COX-2 are associated with a lower risk of serious upper gastro-intestinal side-effects than non-selective NSAIDs.
- Recommendations are that NSAIDs associated with a low risk e.g. ibuprofen are generally preferred, to start at the lowest recommended dose and not to use more than one oral NSAID at a time.
The combination of a NSAID and low-dose aspirin can increase the risk of gastro-intestinal side-effects; this combination should be used only if absolutely necessary and the patient should be monitored closely.
While it is preferable to avoid NSAIDs in patients with active or previous gastro-intestinal ulceration or bleeding, and to withdraw them if gastro-intestinal lesions develop, nevertheless patients with serious rheumatic diseases are usually dependent on NSAIDs for effective relief of pain and stiffness.
- Patients at risk of gastro-intestinal ulceration (including the elderly), who need NSAID treatment should receive gastroprotective treatment.
Systemic as well as local effects of NSAIDs contribute to gastro–intestinal damage; taking oral formulations with milk or food, or using enteric-coated formulations, or changing the route of administration may only partially reduce symptoms such as dyspepsia.
NSAIDs and alcohol
Alcohol increases the risk of gastro-intestinal haemorrhage associated with NSAIDs. Specialist sources recommend that concurrent use need not be avoided with moderate alcohol intake, but greater caution is warranted in those who drink more than the recommended daily limits.
- Some cases of acute kidney injury have been attributed to use of NSAIDs and acute excessive alcohol consumption.
Strong opioids
Morphine remains the most valuable opioid analgesic for severe pain although it frequently causes nausea and vomiting. It is the standard against which other opioid analgesics are compared. In addition to relief of pain, morphine also confers a state of euphoria and mental detachment.
Morphine is the opioid of choice for the oral treatment of severe pain in palliative care. It is given regularly every 4 hours (or every 12 or 24 hours as modified-release preparations).
Buprenorphine has both opioid agonist and antagonist properties and may precipitate withdrawal symptoms, including pain, in patients dependent on other opioids. It has abuse potential and may itself cause dependence. It has a much longer duration of action than morphine and sublingually is an effective analgesic for 6 to 8 hours. Unlike most opioid analgesics, the effects of buprenorphine are only partially reversed by naloxone hydrochloride.
Dipipanone hydrochloride used alone is less sedating than morphine but the only preparation available contains an antiemetic and is therefore not suitable for regular regimens in palliative care.
Diamorphine hydrochloride (heroin) is a powerful opioid analgesic. It may cause less nausea and hypotension than morphine. In palliative care the greater solubility of diamorphine hydrochloride allows effective doses to be injected in smaller volumes and this is important in the emaciated patient.
Alfentanil, fentanyl and remifentanil are used by injection for intra-operative analgesia; fentanyl is available in a transdermal drug delivery system as a self-adhesive patch which is changed every 72 hours.
Methadone hydrochloride is less sedating than morphine and acts for longer periods. In prolonged use, methadone hydrochloride should not be administered more often than twice daily to avoid the risk of accumulation and opioid overdosage. Methadone hydrochloride may be used instead of morphine in the occasional patient who experiences excitation (or exacerbation of pain) with morphine.
Oxycodone hydrochloride has an efficacy and side-effect profile similar to that of morphine. It is commonly used as a second-line drug if morphine is not tolerated or does not control the pain.
Papaveretum is rarely used; morphine is easier to prescribe and less prone to error with regard to the strength and dose.
Pentazocine has both agonist and antagonist properties and precipitates withdrawal symptoms, including pain in patients dependent on other opioids. By injection it is more potent than dihydrocodeine tartrate or codeine phosphate, but hallucinations and thought disturbances may occur. It is not recommended and, in particular, should be avoided after myocardial infarction as it may increase pulmonary and aortic blood pressure as well as cardiac work.
Pethidine hydrochloride produces prompt but short-lasting analgesia; it is less constipating than morphine, but even in high doses is a less potent analgesic. It is not suitable for severe continuing pain. It is used for analgesia in labour; however, other opioids, such as morphine or diamorphine hydrochloride, are often preferred for obstetric pain.
Tapentadol produces analgesia by two mechanisms. It is an opioid-receptor agonist and it also inhibits noradrenaline reuptake. Nausea, vomiting, and constipation are less likely to occur with tapentadol than with other strong opioid analgesics.
Tramadol hydrochloride produces analgesia by two mechanisms: an opioid effect and an enhancement of serotonergic and adrenergic pathways. It has fewer of the typical opioid side-effects (notably, less respiratory depression, less constipation and less addiction potential); psychiatric reactions have been reported.
Weak opioids
Codeine phosphate can be used for the relief of mild to moderate pain where other painkillers such as paracetamol or ibuprofen have proved ineffective.
- Dose - Adult - 30–60 mg every 4 hours if required; maximum 240 mg per day
Dihydrocodeine tartrate has an analgesic efficacy similar to that of codeine phosphate. Higher doses may provide some additional pain relief but this may be at the cost of more nausea and vomiting.
Meptazinol is claimed to have a low incidence of repiratory depression. It has a reported length of action of 2 to 7 hours with onset within 15 minutes.
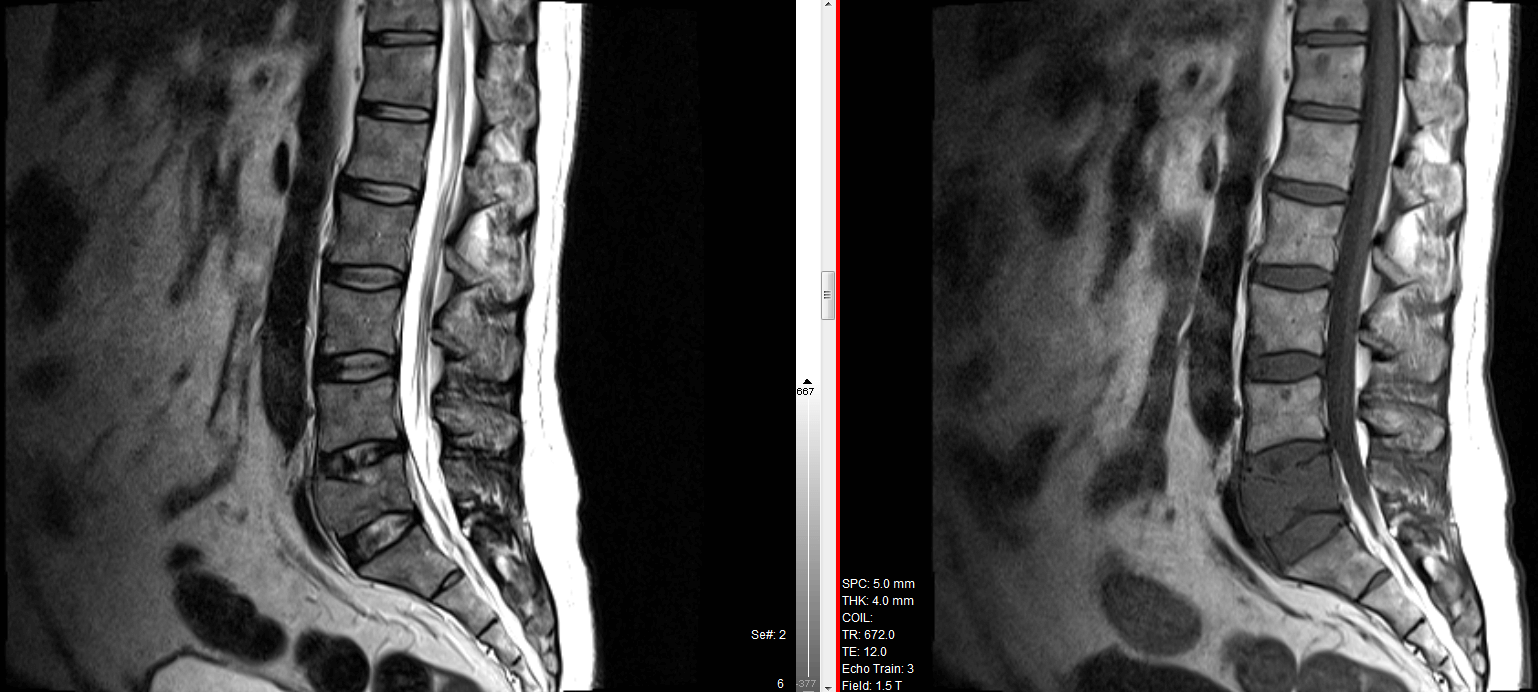
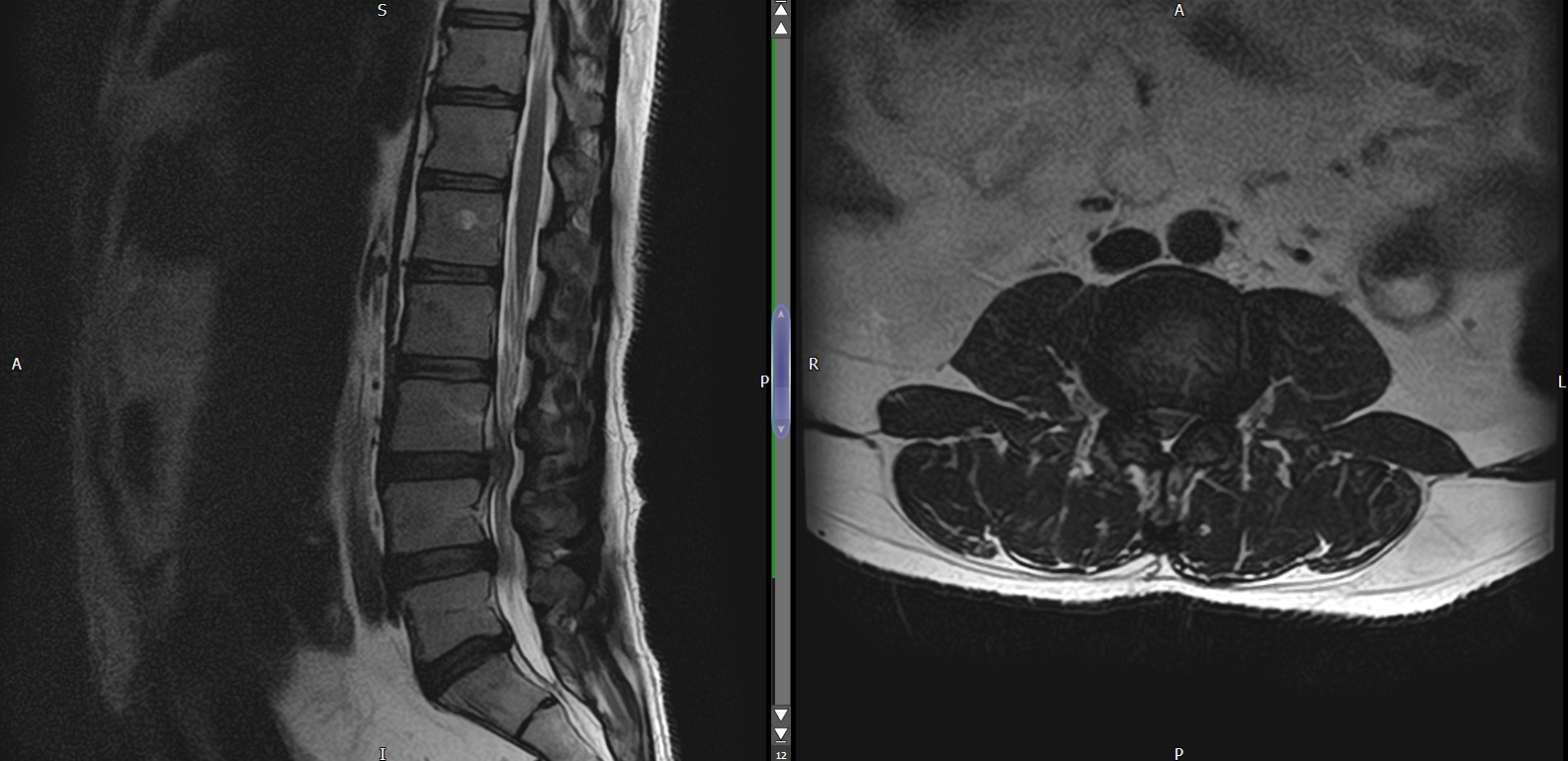
Back Pain & Sciatica
- Consider NSAID for management of acute low back pain.
- A weak opioid, either alone or with paracetamol, can be used to manage acute low back pain only if an NSAID is contra-indicated, not tolerated or ineffective. Paracetamol alone is ineffective for managing low back pain.
- Benzodiazepines (Diazepam) are sometimes used to manage acute low back pain (particularly in loss of lordosis); however evidence to support their use is very weak.
- In patients with chronic low back pain who have had an inadequate response to non-drug treatment, NSAIDs should be considered as first-line therapy. Opioids should be the last treatment option considered and should be considered only in patients for whom other therapies have failed and only if the potential benefits outweigh the risks for individual patients. If indicated, opioids should only be prescribed for a limited period of time. Long term opioid therapy should be avoided.
- Selective serotonin re-uptake inhibitors (SSRIs), serotonin and noradrenaline re-uptake inhibitors (SNRIs), tricyclic antidepressants, gabapentinoids, and antiepileptic drugs should not be offered for managing low back pain.
- When non-surgical treatment is ineffective in patients with moderate or severe localised back pain arising from structures supplied by the medial branch nerve, referral for radiofrequency denervation can be considered.
- Patients with acute and severe sciatica may benefit from treatment with epidural injections of a local anaesthetic and/or corticosteroid.
Non-drug treatment
- Exercise programmes, manual therapy (spinal manipulation, mobilisation, or soft-tissue techniques such as massage), and psychological therapies should be considered for managing low back pain with or without sciatica.
- Spinal decompression may be considered in patients with sciatica when pain and function has not improved with non-surgical treatment (including drug treatment).
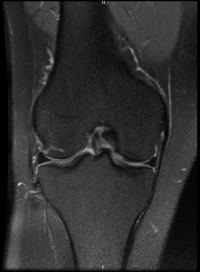
Osteoarthritis
- For pain relief in osteoarthritis, simple analgesia such as paracetamol or a topical NSAID (particularly for hand or knee involvement) is first-line treatment and may need to be used regularly if pain remains uncontrolled. If treatment with simple analgesia is ineffective, consider use of an oral NSAID when required (topical NSAID use should be discontinued), or a weak opioid analgesic (such as codeine phosphate) when required, or topical capsaicin 0.025%, particularly in knee or hand osteoarthritis. In patients taking low-dose aspirin, other analgesic treatment options should be considered before using a NSAID.
- Intra-articular corticosteroid injections can be considered as an adjunctive treatment for relief of moderate to severe pain associated with osteoarthritis.
- Glucosamine, chondroitin, and topical rubefacients (which may contain nicotinate compounds, salicylate compounds, essential oils, and camphor) are not recommended for the treatment of osteoarthritis. Intra-articular preparations of hyaluronic acid and its derivatives are also available for osteoarthritis of the knee, but are not recommended.
Neuropathic pain
Neuropathic pain, which occurs as a result of damage to neural tissue, includes phantom limb pain, compression neuropathies, peripheral neuropathies (e.g. due to Diabetic complications, chronic excessive alcohol intake, HIV infection, chemotherapy, idiopathic neuropathy), trauma, central pain (e.g. pain following stroke, spinal cord injury, and syringomyelia), and postherpetic neuralgia (peripheral nerve damage following acute herpes zoster infection (shingles)). The pain may occur in an area of sensory deficit and is sometimes accompanied by pain that is evoked by a non-noxious stimulus (allodynia).
Neuropathic pain is generally managed with a tricyclic antidepressant or with certain antiepileptic drugs. Amitriptyline hydrochloride and pregabalin are effective treatments for neuropathic pain. Amitriptyline hydrochloride and pregabalin can be used in combination if the patient has an inadequate response to either drug at the maximum tolerated dose.
Nortriptyline [unlicensed indication] may be better tolerated than amitriptyline hydrochloride.
Gabapentin is also effective for the treatment of neuropathic pain.
Neuropathic pain may respond to opioid analgesics. There is evidence of efficacy for tramadol hydrochloride, morphine, and oxycodone hydrochloride; however, treatment with morphine or oxycodone hydrochloride should be initiated only under specialist supervision. Tramadol hydrochloride can be prescribed when other treatments have been unsuccessful, while the patient is waiting for assessment by a specialist.
Patients with localised pain who are unable to take oral medicines may benefit from topical local anaesthetic preparations, such as lidocaine hydrochloride medicated plasters, while awaiting specialist review.
Capsaicin is licensed for neuropathic pain (but the intense burning sensation during initial treatment may limit use). Capsaicin 0.075% cream is licensed for the symptomatic relief of postherpetic neuralgia. A self-adhesive patch containing capsaicin 8% is licensed for the treatment of peripheral neuropathic pain. It should be used under specialist supervision.
A corticosteroid may help to relieve pressure in compression neuropathy and thereby reduce pain.
Neuromodulation by spinal cord stimulation may be of benefit in some patients. Many patients with chronic neuropathic pain require multidisciplinary management, including physiotherapy and psychological support.