Greater Trochanter Pain Syndrome (GTPS)
GTPS is a painful condition affecting the lateral hip and is thought to have a similar influence on quality of life in comparison to hip OA. It is often diagnosed as trochanteric bursitis, however radiological and surgical studies have revealed that the most common pathology is gluteus medius/minimus tendinopathy +/- bursitis (Kong et al 2007, Bird et al 2001, Kingzett-Taylor et al 1999). Long et al (2013) highlighted <20% of cases have bursal involvement.
Epidemiology: It most commonly affects people aged >40yrs and is 2.4 - 4 times more prevalent in women (Grimaldi & Fearon, 2015). GTPS is thought to have an incidence of 4.22 per 1000 patients and is more common than achilles tendinopathy (in a dutch study by Albers et al 2016). Many people with GTPS continue to experience hip pain (including due to GTPS) and appear to have a higher chance of developing hip OA 11 years later (Bicket et al 2021).
Risk Factors: a) Coxa Vara (greater compressive load on tendon), b) women >40yrs, c) ? some links with obesity, d) LBP e) post-menopause f) sudden increase in training load/volume.
Subjective Clues: Patients will often report lateral hip/thigh pain that is often worse with: a) side lying, b) cross-legged sitting, c) stairs/hills, d) prolonged walking. Approx 35% of GTPS patients also appear to have concomitant LBP.
Tests: Grimaldi et al (2017) recommended a battery of tests in addition to subjective history to aid diagnosis. They stated that pain on palpation over the greater trochanter was the most sensitive test and if included alongside another more specific test such as FADER with resisted IR helped with clinical diagnosis.
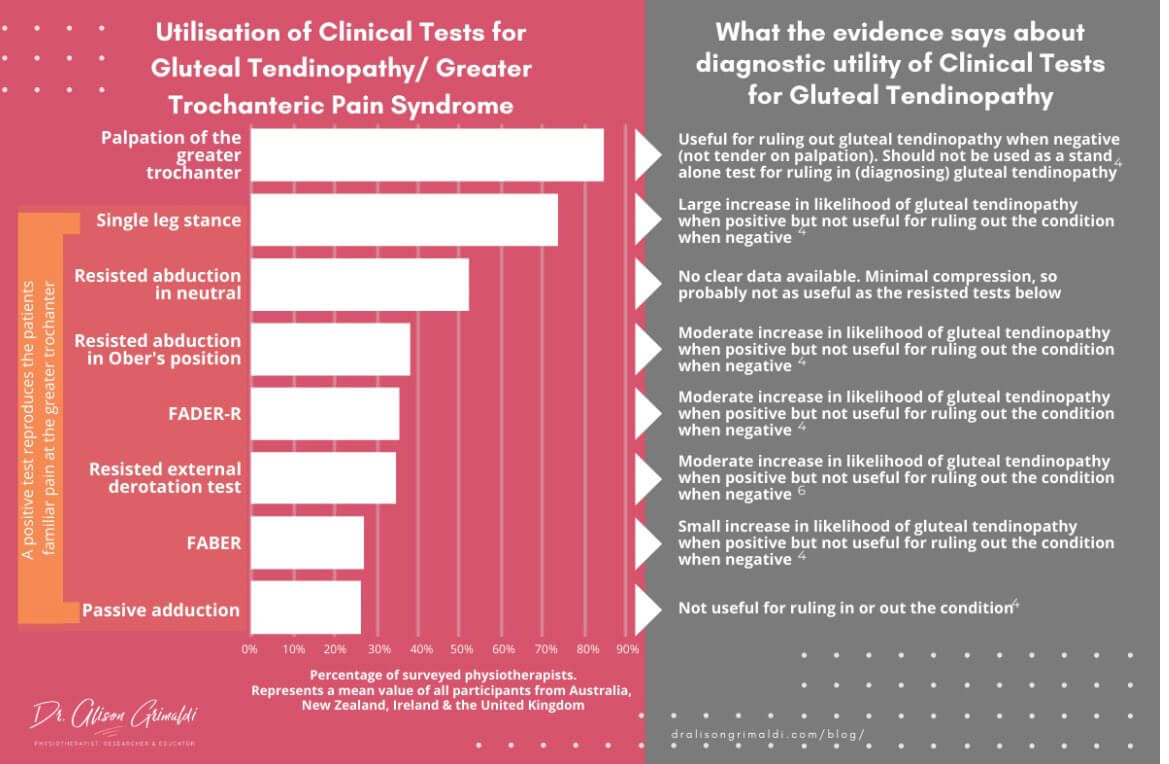
Other tests include; ADD-R, passive hip adduction, FABER, FADER, Single leg standing for 30s (100% sensitivity) are all useful to apply both tensile and compressive loads over the gluteal tendons.
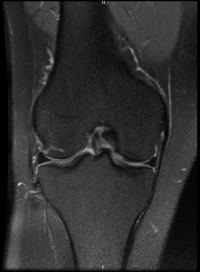
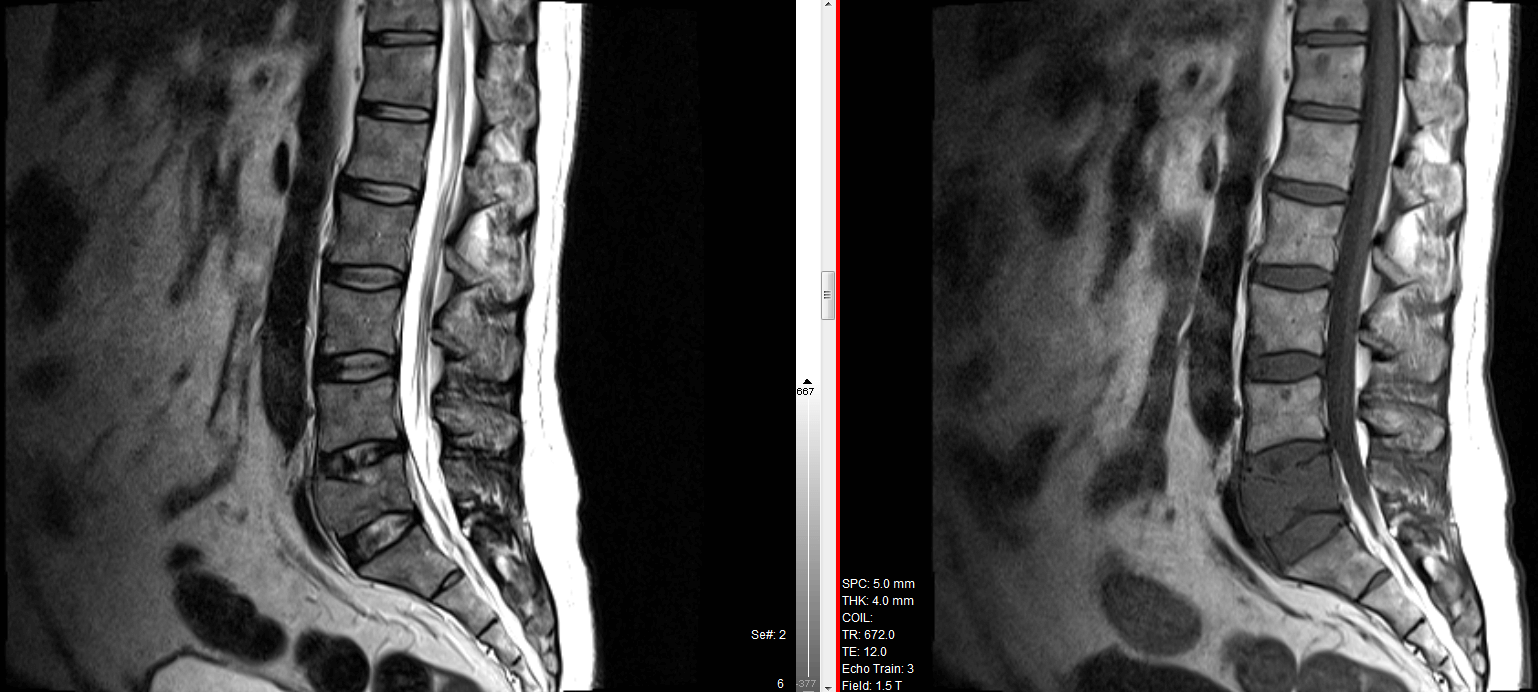
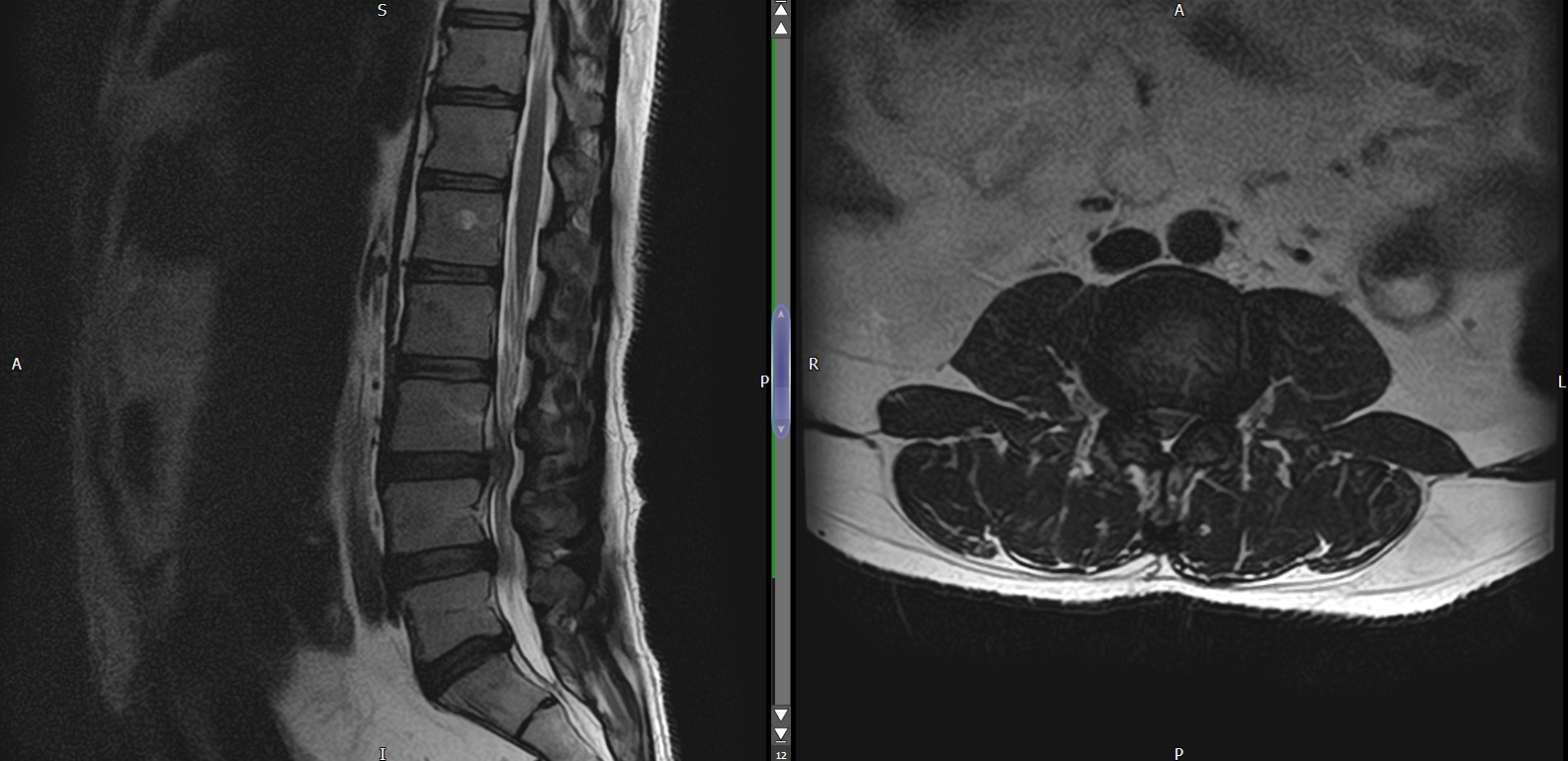
Imaging: Rarely warranted, XR excludes intra-articular pathology if clinician is unsure. US & MRI have good sensitivity & specificity for assessment of gluteal tendon changes and bursal involvement. Blankenbaker et al (2008) found that up to 88% of asymptomatic patients have structural changes on MRI.
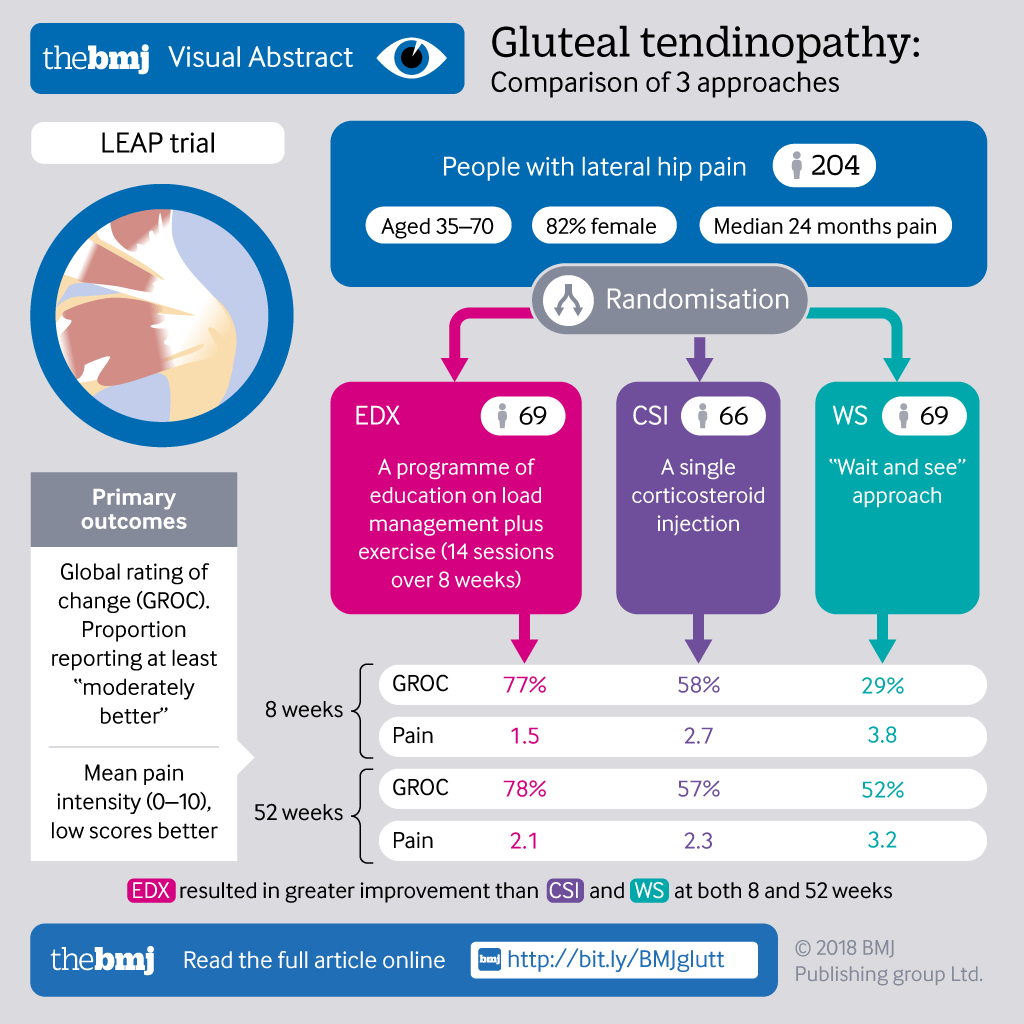
Treatment: The LEAP Trial by Mellor et al (2018) appeared to highlight how clear, concise instructions around the aetiology of the condition, load management and temporary reduction in compressive led to improvements in the exercise and education group.
Cowan et al (2021) demonstrated how the type of exercise doesn’t appear to play a significant role. They compared a GLoBE exercise protocol vs a sham group and found no difference at both 12 weeks and 1year follow up.
Menopause + GTPS: Oestrogen has been shown to have anabolic effects on tendon health. A reduction in oestrogen alters collagen synthesis & tendon strength whilst also increasing low grade, systemic inflammation. Hormone therapy may help improve GTPS symptoms coupled with exercise for patients with 25 BMI. However, it’s effects in overweight / obese patients were no more effective than sham (Cowan et al., 2021).