Atraumatic monotraumatic joint pain
Inflammatory – can be caused by
– microcrystals (gout & pseudogout)
– microorganisms (septic arthritis)
– autoinflammatory (RA)
– reactive arthritis
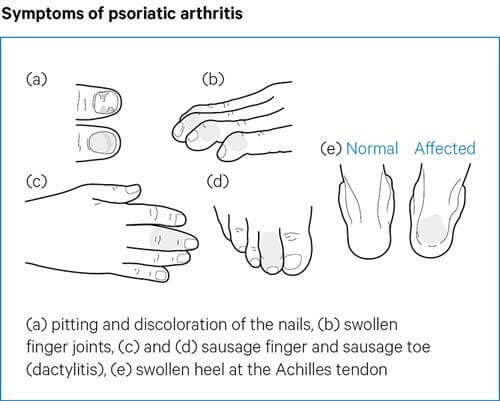
– spondyloarthritis
Mechanical OA
Epidemiology
- Inflammatory monoarthritis affects men > women (because gout is more common in men)
- Most common joint -> Knee
- Crystal arthritis is the most common diagnosis followed by reactive arthritis, RA Septic arthritis.
- Most important diagnosis to exclude is septic arthritis. Risk factors are RA, OA, Prosthetic joints, low socioeconomic status, IV drug abuse, alcoholism, diabetes, previous intra-articular CSI, HIV, cutaneous ulcers. Most common organism is staph aureus followed by staph pyogenes.
- Redness over skin is highly suggestive of either crystal arthritis or septic arthritis.
Onset
- Gout & Pseudogout – acute onset (usually over hours to days).
- Septic arthritis – 1-2 weeks.
Investigations
For acute non traumatic inflammatory monoarthritis
– plain radiograph
– arthrocentesis / synovial fluid analysis (this also excluded septic arthritis)
Lab tests
– FBC (to assess total white cell count and neutrophil count). Total white cell count can be normal in initial presentation in septic arthritis. CRP is a more reliable predictor in this context.
– CRP, ESR
– Liver function (important in management decisions)
– blood culture (in suspected septic arthritis) before initiation of antibiotic therapy.
– serum uric acid levels. These fall during an acute systemic inflammatory response. So they are not helpful to exclude gout if they are low.
– Arthrocentesis. Joint fluid analysis, gram staining and culture.
– Polarised Light Microscopy – demonstration of microcrystals in synovial fluid is gold standard for crystal arthritis.
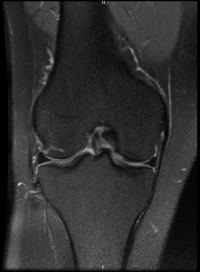
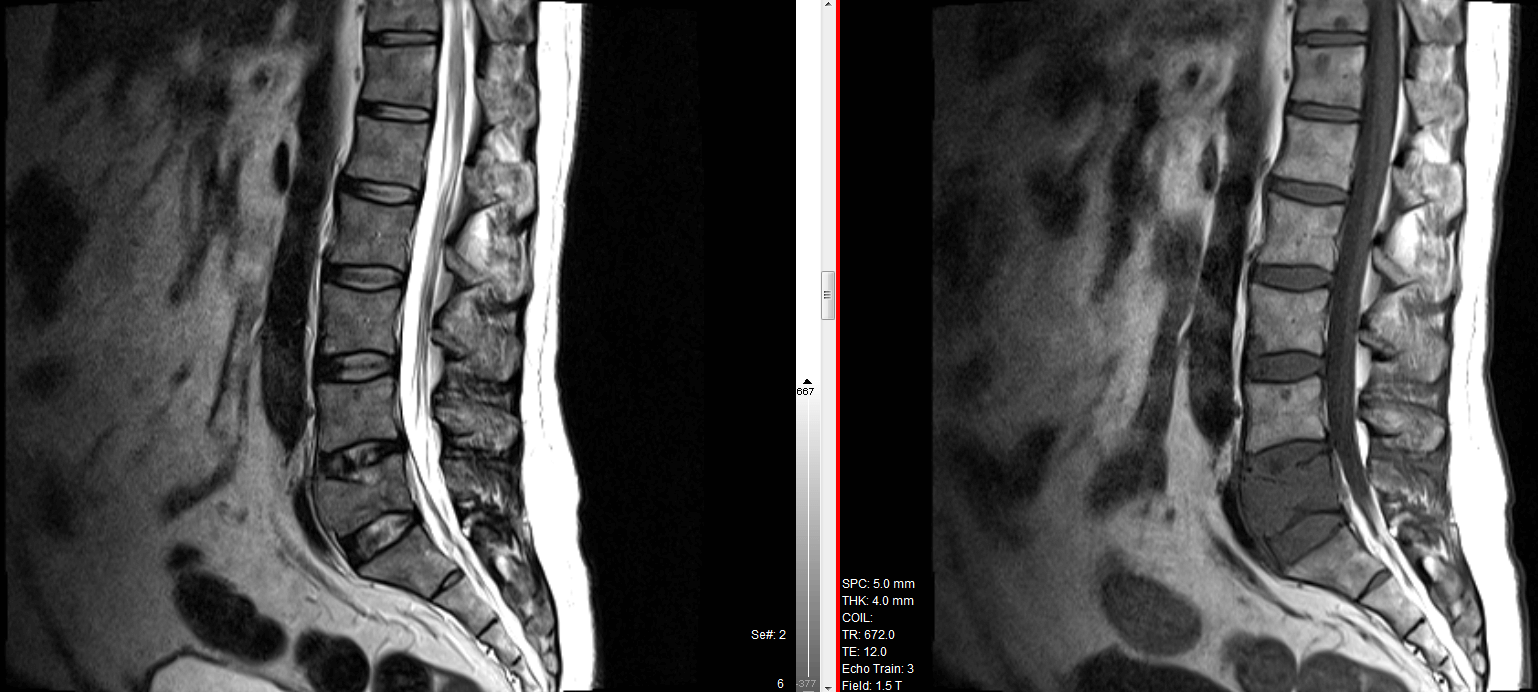
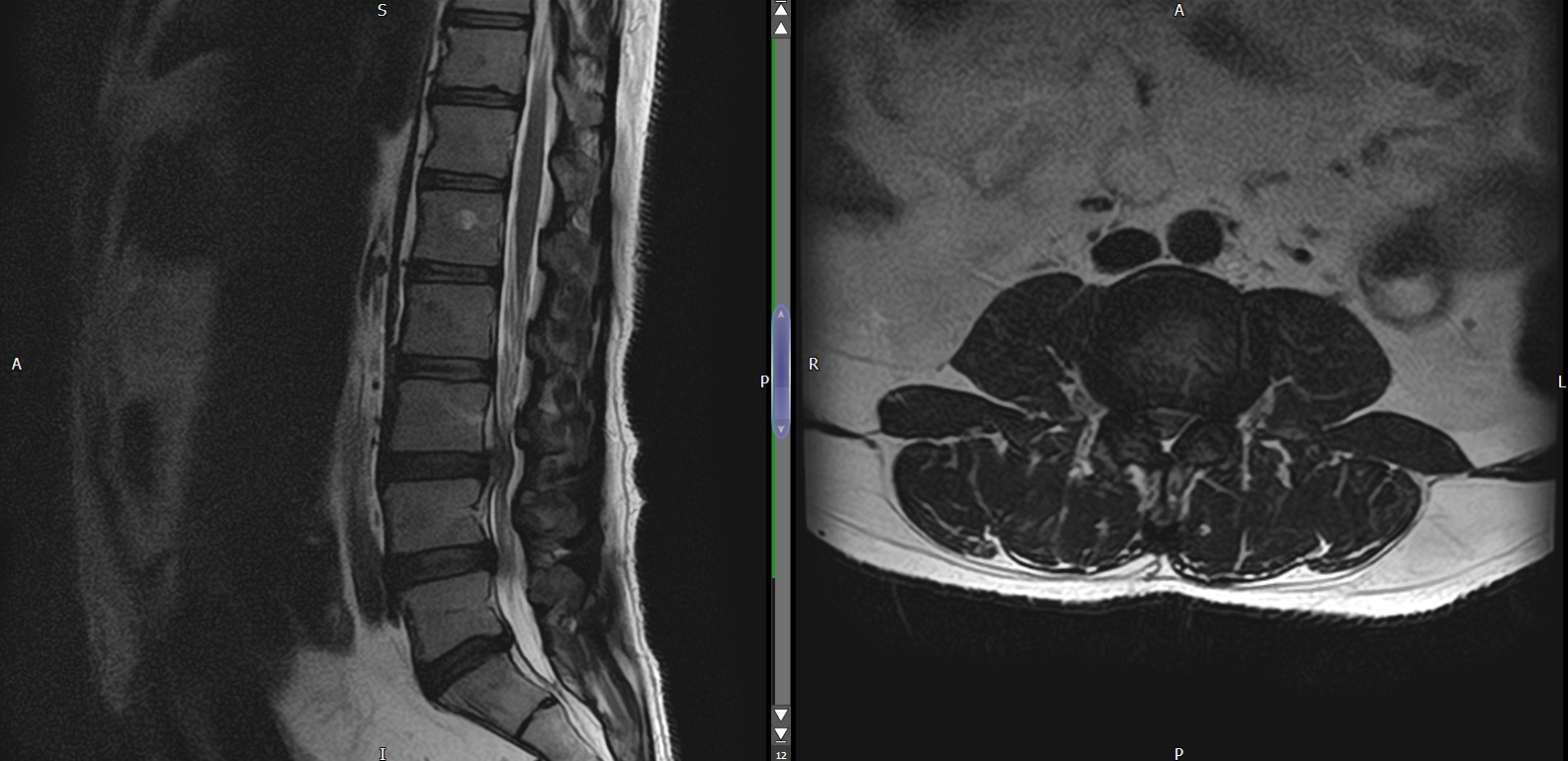
Radiology – X-ray, MRI
– helpful to diagnose AVN, heamochromatosis, PVNS
Supplementary Investigations
– arthroscopic biopsy of synovium in case it persists beyond several weeks.