Tissue injury may be caused by trauma, heat, chemicals, bacteria etc.. Any injury causes a release of substances by the injured tissue which causes a local change or a reaction in the injured tissue and its vicinity. This is called inflammation. This is characterised by the following elements.
- Vasodilation of local blood vessels causing an increased blood flow.
- Increased permeability of capillaries allowing leakage of fluid in to the interstitial spaces.
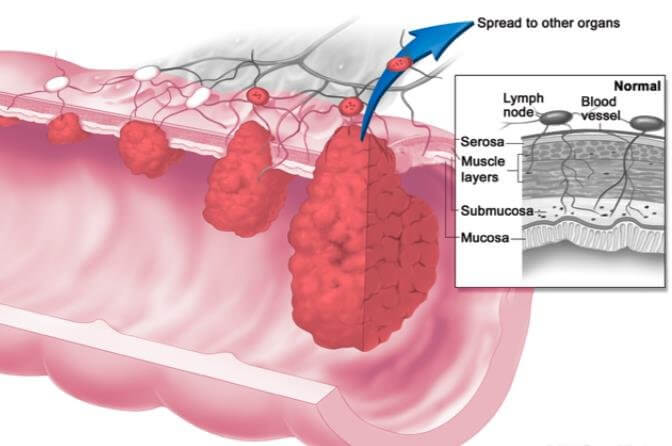
- Clotting of fluid in the interstitial spaces due to fibrinogen and other proteins leaked from capillaries. This causes a “walling off” effect by blocking the interstitial spaces and lymphatics as it blocks any flow of fluid to and from the area. This stops or slows down the spread of bacteria / toxin to other sites.
- Migration of granulocytes and monocytes to the injured tissue site.
- Swelling of the tissue cells.
The main substances which are involved in these reactions are histamine, bradykinin, serotonin, prostaglandins, lymphokines and various other products of complement and blood clotting systems.
The macrophages are activated to eat away the dead tissue or the invading organism.
Role of Macrophages and Neutrophils during Inflammation
Local Macrophages – Tissue macrophages are the first line of defense against infection. Very soon after inflammation / infection begins i.e within minutes, macrophages enlarge rapidly and begin phagocytic action. These could be histiocytes (epithelial macrophages), alveolar macrophages, microglia etc.
Neutrophil Invasion (second line of defense) – within the first hour a large number of neutrophils are attracted to the inflamed area triggered by various mediators of inflammation like cytokines.
Neutrophilia – Sometimes the number of neutrophils in blood increase 4-5 fold from 4000 – 5000 to 20000 per microlitre called neutrophilia. The mediators of inflammation reach the bone marrow via blood and mobilise the stored neutrophils in to circulating blood so as to reach the inflamed tissue.
Macrophage Invasion (third line of defense) – along with the neutrophils, monocytes also enter the blood and enlarge to become macrophages once they reach affected tissue. They are still immature and take up to 8 hours to increase in size and develop lysosomes and then only they develop phagocytic capability. They are low in number compared to neutrophils. Hence their buildup in the tissue is slower, but after a few days macrophages are the predominant phagocytic cell owing to increased production of monocytes in the bone marrow. Macrophages can phagocytize greater number of bacteria and larger particles compared to neutrophils.
Increased production of Granulocytes and Monocytes (fourth line of defense) – Stimulation of granulocytic and monocytic progenitor cells in the bone marrow causes an increased production of granulocytes and monocytes which can continue to happen for weeks or months or even years if the stimulus from injured tissue continues. It takes 3-4 days before these newly formed granulocytes and monocytes can leave the bone marrow to reach the target site.
Factors causing increased production of Macrophages and Neutrophils
- Tumour Necrosis Factor – TNF
- Interleukin – 1 IL1
- Granulocyte-monocyte colony-stimulating factor – GM-CSF
- Granulocyte colony-stimulating factor – G-CSF
- Monocyte colony-stimulating factor – M-CSF
These factors are formed by activated macrophages in the inflamed tissue.
Role of Eosinophils
Eosinophils are weak phagocytes and therefore not significant in protection against normal infections. They are produced in large numbers in parasitic infections. As most parasites are too large to be phagocytized, eosinophils attach to them and release substances that kill them.
Role of Basophils
Basophils are similar to mast cells in that they release heparin apart from histamine, bradykinin and serotonin. They play some role in allergic reactions.