Total Blood Volume (TBV) = 8% of body weight in kg. e.g. someone weighing 70 kg will have 0.08 x 70 kg = 5.6 kg = 5.6 Litre blood.
Haematocrit (HCT) – take sample of blood and spin it in a centrifuge. Heavier things settle to the bottom i.e. blood cells, and lighter plasma rises to the top.
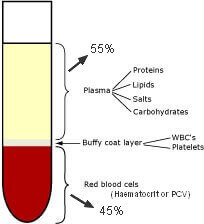
Plasma = 55%
Haematocrit = 45%
WBC + Platelet layer = Buffy Coat
- Haematocrit is also called Packed Cell Volume (PCV). Most of these are RBCs.
- Normal HCT is 45%
- HCT < 45 is anaemia
- HCT > 45 is Polycythemia. Poly = many, Cyt = cells, Hemia = “in the blood”. Many cells in blood = Polycythemia.
- People living at higher altitudes where there is less oxygen have some degree of polycythemia to compensate for lack of oxygen. Athletes train at high altitude to increase RBCs.
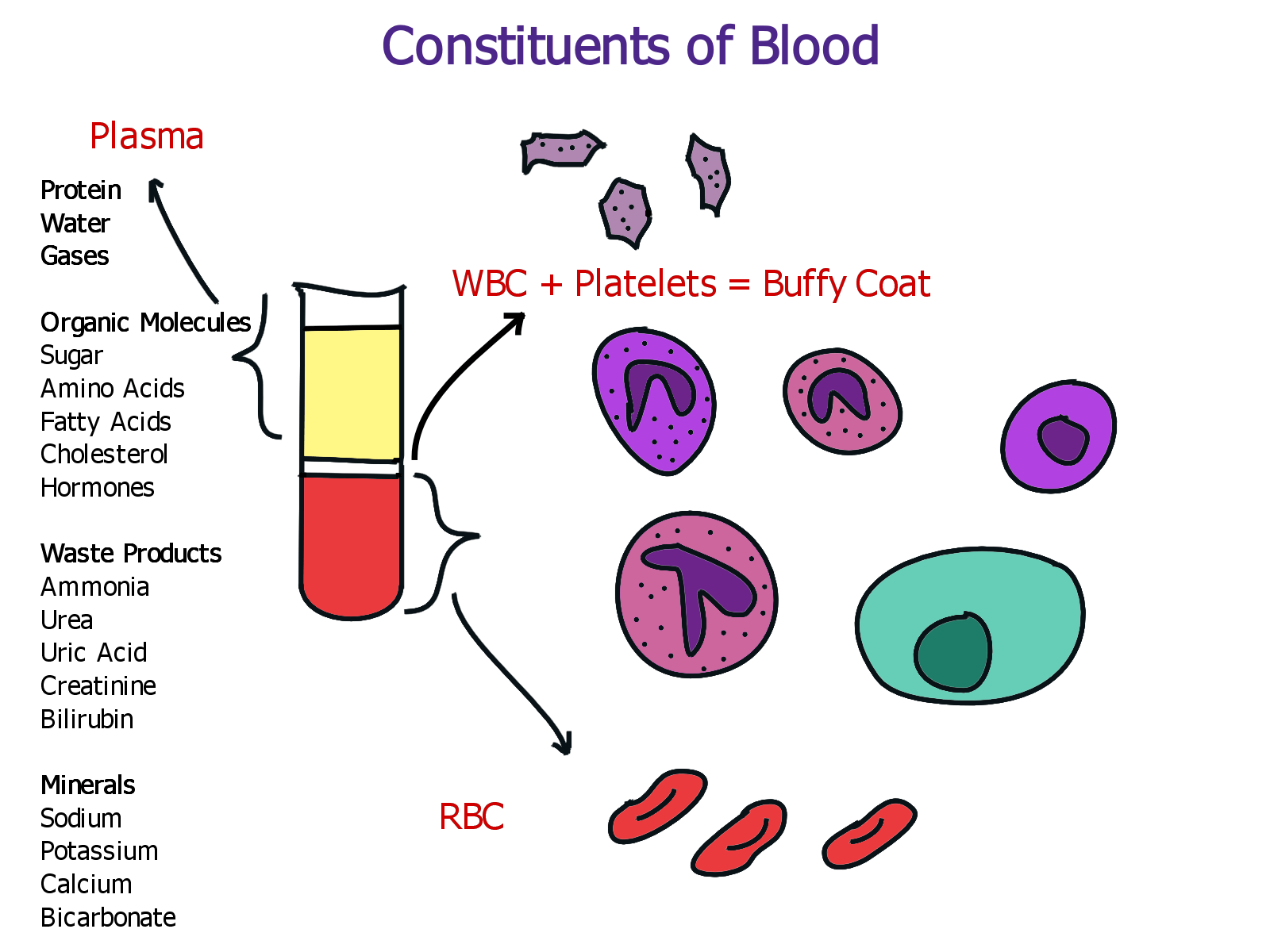
Composition of Blood Plasma
- 90% water
- Solute (these are dissolved in water)
Protein
- Normal amount of protein is 7% which = 7g/100 ml or 7g / decilitre of blood.
- Most of the proteins are synthesised in liver. These are of various types.
- Proteins are analysed by Electrophoresis.
- Phoresis = separate. Separation using electrical field = Electrophoresis.
- Most proteins have a negative polarity so they are attracted to the positive electrode. Some move faster than other. Lighter proteins move faster. This separates the proteins into different groups.
- Albumin moves the fastest as it has low molecular weight.
- Globulin = means proteins. These are groups or clusters of protein. They are of different types. These are alpha Ɑ (alpha 1 and alpha 2), Beta and Gamma Ɣ.
- HDL is a type of Alpha 1 globulin
- LDL is a type of Beta Globulin
Albumin
- Albumin is 60% of plasma protein.
- It is needed for maintaining colloid osmotic pressure (COP). These draw water from tissues into the blood stream. BP forces blood out of the capillaries. So if protein is low, it would lead to oedema.
Globulin
- Globulin is 35% of plasma protein.
- Alpha and Beta globulins transport fats including cholesterol, and certain minerals in blood stream including iron.
- Fats cannot dissolve in water, so to move them, they are attached to proteins and proteins carry them in blood stream. So all fats are bound to proteins. These proteins which transport fats are called Lipoproteins.
- Transferrin is an beta globulin which transports iron.
- Ceruloplasmin is an alpha globulin which transports copper.
Lipoproteins
- HDL – High Density Lipoproteins is an alpha globulin
- LDL – Low Density Lipoprotein is a beta globulin.
- Both are made in liver. They both carry cholesterol.
- Good and bad cholesterol is a misnomer. There is a good and bad lipoprotein.
- LDL – (Lethal) – transports the cholesterol from liver to arterial walls. Cholesterol is used by cells to manufacture steroid hormones. If LDL level is high, one will transfer more cholesterol to the arterial walls. Levels of LDL are determined by genes. Some make more and some less.
- HDL (Healthy) – transports cholesterol back to liver from arterial walls.
Gamma Globulins
- Gamma Globulins = Antibodies (Ab) = Immunoglobulins (Ig)
- These proteins are made in Lymphocytes.
- Antibodies are made by B lymphocytes.
- Immunoglobulins are of 5 types. IgG, A, M, D, E.
- Most of the antibodies are IgG. These attack bacteria and viruses.
- IgE are in trace amounts. These act on allergens.
Blood Clotting Proteins
- These are 5% of plasma proteins.
- This includes prothrombin and fibrinogen.
Serum = Plasma minus clotting factors.
So if you put plasma in a glass beaker, it will form a clot on the top. These are all the clotting factors. If you remove that clot, you have serum.
Advantages of Serum
Infusing whole blood or plasma in a patient can cause blood clots because it has clotting factors. So heparin has to be infused in the IV line to flush it to prevent blood clots. With serum infusion, there is no risk of blood clots.
Haemophilia = genetic inability to form clotting proteins.
In addition to proteins, what else is in plasma?
Organic molecules
- Sugar – 100 mg / decilitre in blood
- Amino accids
- Fatty acids
- Cholesterol – normal < 200mg / dl
- Hormones – measured in micrograms (thyroxine, cortisol, estrogen, PTH, calcitonin, renin, aldosterone, FSH, LH etc.). These are measured using radioimmune assay.
Waste products
- NH3 – Ammonia
- Urea (BUN)
- Both Ammonia and Urea is formed by deamination of amino acids by liver. Proteins are broken down into amino acids. Then amino group is removed forming ammonia. liver converts ammonia into urea. This is re-released into the blood. Then kidney excretes it.
- Uric acid – formed by breakdown of nucleotides. High uric acid -> gout
- Creatinine – waste product formed in muscles.
- Bilirubin – formed by breakdown of RBCs.
Minerals
- Sodium – normal 150 mEq/L
- Potassium – normal 5mEq/L
- Calcium – important for muscle contraction and blood clotting.
- Bicarbonate – Acts as buffer.
Blood Cells
There are 3 main kinds of cells or formed elements.
- RBC – most abundant. 5 million per cubic mm = 5 x 106 / mm3
- WBC – 7000 per cubic mm = 7×103 / mm3
- Platelets / Thrombocytes
RBC | Erythrocytes
These are among the smallest cells in the body. 0.8 µm in diameter. The only other cell smaller than RBC is a sperm. For comparison, a normal liver cell, pancreatic cell or kidney cell is 100 µm. Small size allows them to move through capillaries.
- RBCs don’t have a nucleus. When they are formed they have a nucleus but when they are released in blood, the nucleus breaks down.
- life span is 4 months (120 days).
- Because they have no nucleus, they have no genetic information, so they can’t repair themselves.
- Most RBCs are made in vertebral coloumn including sacrum and pelvis, sternum and rib cage bone marrow.
- RBCs are produced in long bones such as tibia and femur before birth and in the early years. By the age of 20-25 years, the RBC production in femur, tibia is down to zero. The red marrow gets replaced by fat or yellow marrow.
ABO Blood Types
Cell membranes have proteins which act as recognition sites that allows WBCs to recognise what cells are our own and what are foreign. These are called cell identity markers, recognition sites or Major Histocompatibility complex (MHC).
- RBCs have 2 major MHC sites. One is for A or B protein, the other is for Rh protein.
- RBCs either have “A” protein or “B” protein or no protein called as “O”.
- The other group is Rh protein. It is either +ve or -ve.
- 80% of population is Rh +ve.
Normally one has to be exposed to something foreign in order to produce antibodies. But our bodies naturally produce antibodies to the blood group that we are not.
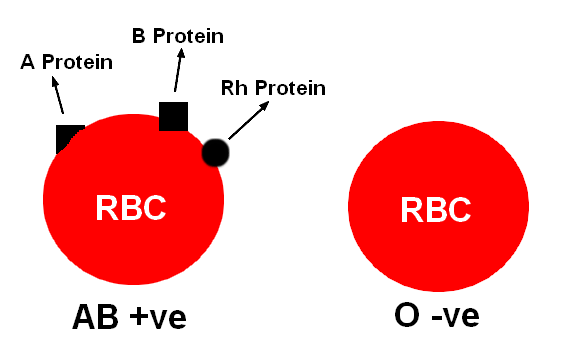
The RBC on the left has A protein, so it will not produce antibodies against “A” protein. Similarly it has “B” protein, so it will not produce antibodies against B protein. Likewise it has Rh protein, so it will not produce antibodies against Rh protein. So this person doesn’t have antibodies against RBCs. This is AB+ve and is called universal recipient and can take any blood.
In the O-ve RBC, it doesn’t have A or B protein, so it will produce antibodies against A & B proteins. It doesn’t have Rh protein, so it will produce antibodies against Rh protein.
Erythroblastosis Foetalis – Mother is Rh-ve and the child is Rh+ve, so mother produces antibodies against the foetus.
Genetics of ABO blood types
ABO blood groups are controlled by gene I. This gene has 3 alleles IA, IB, i. The alleles IA and IB produce a slightly different form of sugar while allele i doesn’t produce any sugar.
The plasma membrane of RBCs has sugar polymers which protrude from its surface and the kind of sugar is controlled by the gene. Because humans are diploid organisms each person possesses any 2 of the 3 I genes. IA and IB are dominant over i. When IA and i are present, IA expresses because i doesn’t produce any sugar. But when IA and IB both are present, both express their own types of sugars because of co-dominance.
RBCs Contd.
- Normal level of RBC = 5 million per cubic mm = 5 x 106 / mm3
- Low RBC = Anaemia
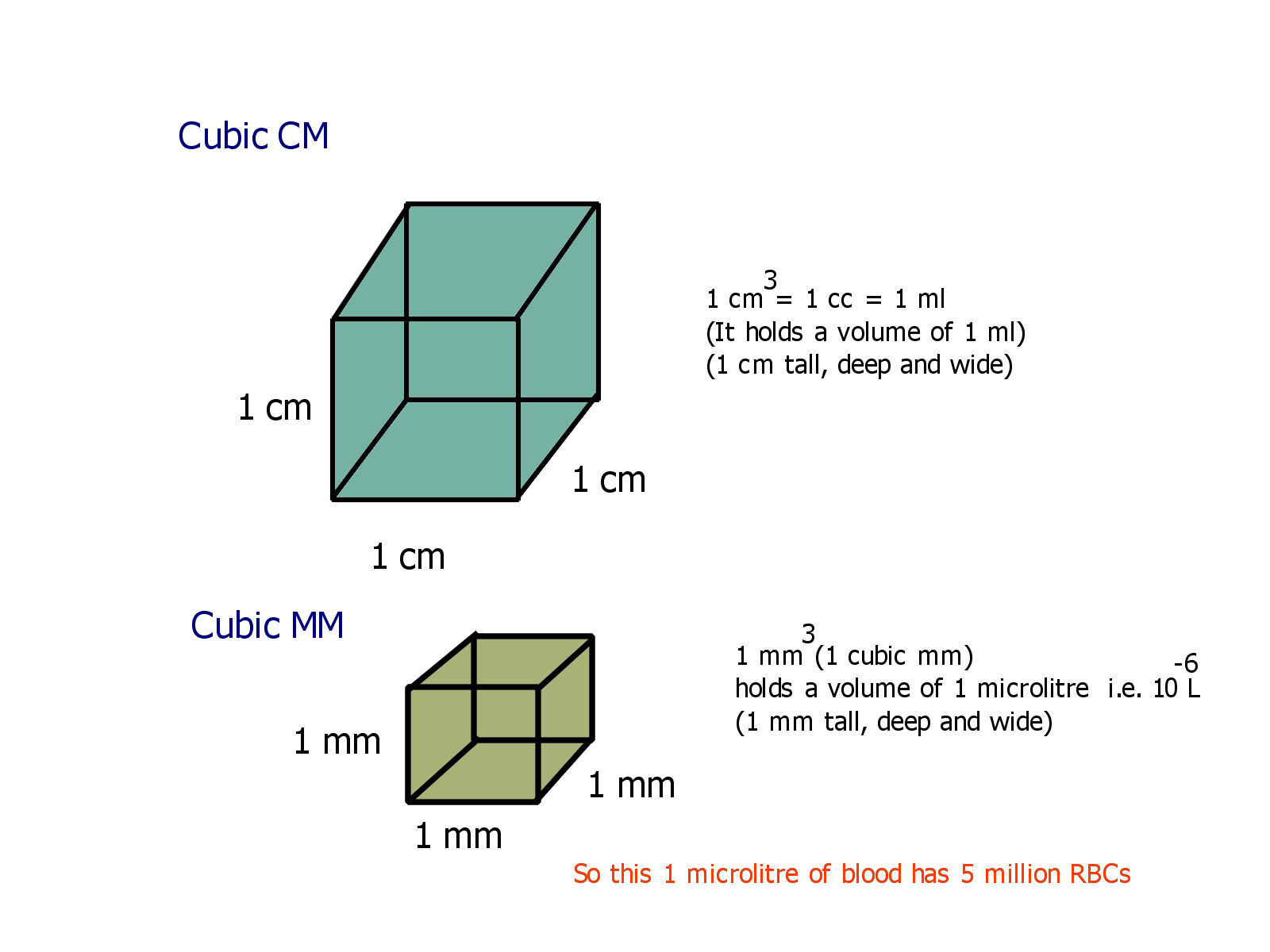
- 1 cm3 = 1cc = 1 ml i.e. it holds a volume of 1 ml
- If someone needs 5 ml of a drug, it might be mentioned that they need 5 cc of a drug.
- 1 mm3 = 1 cubic mm. It holds a volume of 1 microlitre (µL) i.e. 10-6 L
- 1 µL of blood contains 5 million RBCs.
- 2 million RBCs are dying every second and 2 million are made every second.
Erythropoietin
- Erythropoietin is secreted by kidneys. It is a hormone that stimulates erythropoiesis or formation of RBCs in bone marrow.
- Erythropoietin hormone is given to people who have failing kidneys as they cannot produce enough erythropoietin.
- It is also given to people undergoing chemotherapy because chemo damages bone marrow. Damage to bone marrow causes a drop in RBC, WBC and Platelets.
RBC – Life span
RBCs only live for 4 months because they have no nucleus and thus no genetic material. RBC is a very small cell and if it had a nucleus it would not be able to carry any oxygen.
Old and damaged RBCs are removed from blood stream by macrophages especially in spleen and liver. They are broken down into heme and globin. Globin is a protein and broken down in to amino acids. From heme iron is removed and what is left is bilirubin. The bilirubin is secreted by liver with bile. Iron (Fe2+) is recycled back to bone by protein transferrin (made by liver) which is a transport protein in blood.
Anaemia
Anaemia = Reduced number of RBCs. This reduces oxygen in blood. Therefore the ability of cells to carry out aerobic cellular respiration reduces. This causes reduced production of ATPs. Therefore people with anaemia feel tired because they produce less ATPs. They also feel cold because cellular respiration is the major source of heat production in our body.
Haemoglobin
Normally it is 15g/100 ml = 15%
It is also measured along with RBCs because sometimes one can have normal RBCs but reduced Hb. Reasons below.
- Iron deficiency anaemia
- Vit B12 deficiency anaemia (Pernicious anaemia)
- Folic Acid deficiency anaemia
- Aplastic anaemia – occurs with chemotherapy due to degeneration of bone marrow.
- Sickle cell anaemia – RBC is misshapen. It is a genetic disorder.
Platelets (Thrombocytes)
- Megakaryocytes are cells in bone marrow. They break off pieces of cytoplasm into the blood stream. These are platelets. So platelets are pieces of cells.
- A hormone called thrombopoietin stimulates the production of platelets in bone marrow. This hormone is produced by liver.
- Thrombocytopenia – lower number of thrombocytes.
- Affects the ability to form blood clots.
- Therefore someone undergoing chemotherapy not only has anaemia but also has thrombocytopenia because of damage to bone marrow.
Haemostasis
Control of bleeding = Haemostasis
When a blood vessel is injured, there are 3 steps which are as follows.
1. Vascular Spasm – The blood vessel spasms. This is mediated by a chemical called thromboxane A2. This causes vasoconstriction & platelet aggregation.
2. Formation of platelet plug – At the site of injury the platelets aggregate and form a plug. These thrombocytes then release a factor called ‘Platelet Factor’ (PF). This causes formation of a fibrin clot. The thrombocytes are attracted to rough edges of a blood vessel where they aggregate and then release PF.
- Aspirin stops the aggregation of platelets. Why do we want this to happen?
- In blood vessels which have atherosclerosis, they have rough interiors. Platelets adhere and aggregate at these sites and release PF which stimulates the formation of a fibrin clot which causes heart attack if they are in coronary vessel or a stroke if in cerebral vessel.
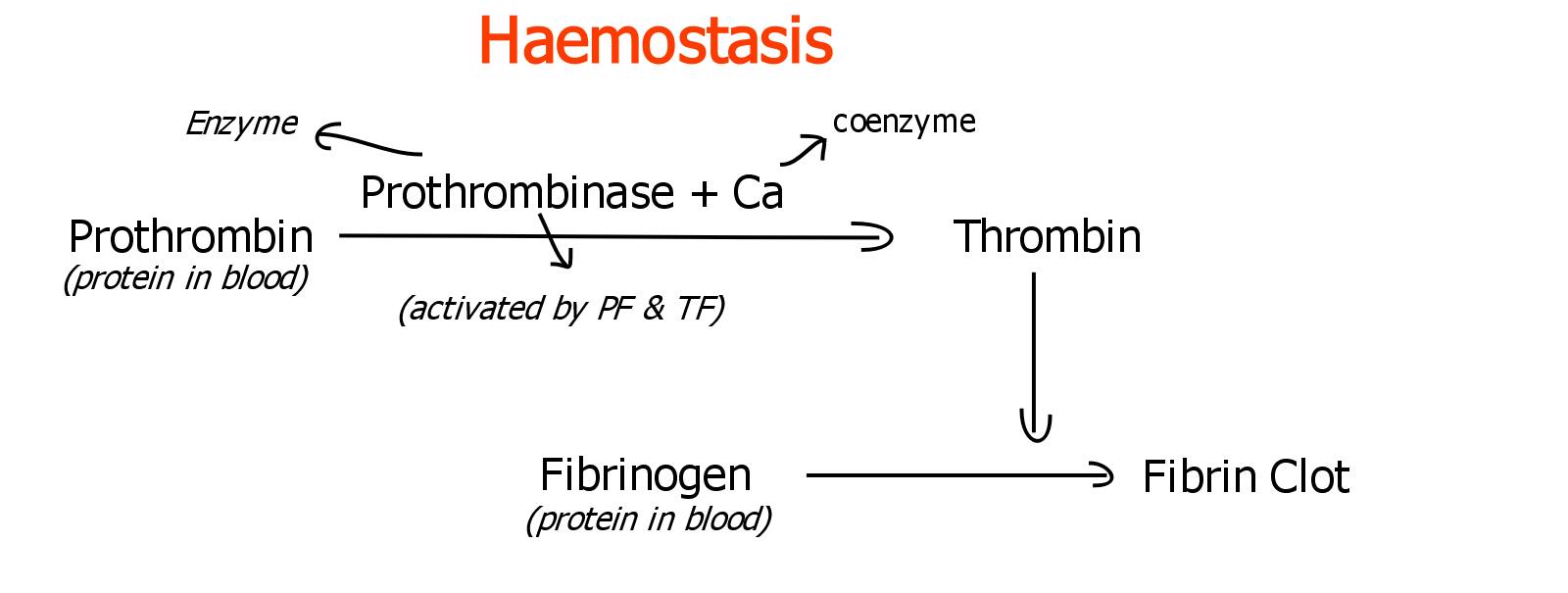
3. Formation of Fibrin Clot (Coagulation) –
- Intrinsic Pathway – The aggregate of platelets release ‘Platelet Factor’ (PF). Injured tissue cells release ‘Tissue Factor’ (TF).
- Extrinsic Pathway – Both PF and TF activate a protein in our blood called prothrombinase (made by liver). This is actually and enzyme. Now prothrombinase along with Ca2+ (which acts as a coenzyme) converts another protein called prothrombin to thrombin.
- Thrombin converts another protein in blood called fibrinogen into a fibrin clot.
Fibrinolysis
When the vessel wall is repaired, the cells in the wall release a chemical called TPA (tissue plasminogen activator). This TPA activates a protein circulating in blood called plasminogen and converts into Plasmin. Plasmin dissolves the fibrin clot. This is called fibrinolysis.
WBCs (White Blood Cells / Leukocytes)
Normal level – 7000 / mm3 or 7 x 103
- Neutrophils – small phagocytes 60%
- Lymphocytes – immune response 25%
- Monocytes – large phagocytes (macrophages)
- Eosinophils – these phagocytise allergens
- Basophils – release Histamine and Heparin. Histamine is a mediator in inflammation.
WBCs are nucleated cells that behave like amoebae. They move out of blood vessels and look for suspicious characters. RBCs do not move on their own. They are only moved by blood pressure.
Leukopenia – lower number of WBCs. Chemotherapy causes leukopenia as it causes thrombocytopenia because it damages teh bone marrow.
Leukocytosis – Higher number of WBCs. Most common reason for this would be someone fighting infection.
WBC Types
2 types. Granular Leukocytes and Agranular Leukocytes
Most cells in our body are transparent, so these are stained or dyed so that they show up better. RBCs are red so they don’t need dyeing. 2 dyes are used for staining blood. These are Haemotoxylin and Eosin.
When WBCs are stained, Neutrophils, Basophils and Eosinophils get stained due to granules. These granules are vacoules. Therefore these are called granulocytes. These vacoules pick up the dye. WBCs also have multilobed nucleus.
Monocytes and Lymphocytes (B & T lymphocytes) are called Agranulocytes. It is not that they don’t have vacoules. They do have them but they don’t take up the dye. This helps to differentiate between the two groups.
Granular Leukocytes
- Possess granules (vacoules) in the cytoplasm.
- Possess a multilobed nucleus. This is why they are also called Polymorphonuclearcytes – PMNs or Polys.
- All are made in bone marrow where RBCs and platelets are made
- Most of the Polys are Neutrophils.
Neutrophils (small phagocytes)
- 60% of total WBCs
- Phagocytise foreign agents
- Neutropenia – low count of neutrophils. Reason – chemotherapy
- Neutrophilia – higher than normal neutrophils. Reason – fighting and infection especially bacterial.
Eosinophils
- Eosinophils phagocytise allergens.
- Eosinophilia – higher than normal eosinophils. This is seen in allergic reactions. They are there to swallow up allergens.
Basophils
- Basophils release histamines. Histamine is a mediator in inflammation.
- Basophils release heparin which is an anticoagulant.
- These are very few in number.
Monocytes
- Largest of all lymphocytes
- Act as macrophages
Lymphocytes
- Smallest amongst WBCs. These are only slightly bigger than RBCs.
- They have very large nucleus
- These are 25% of total WBCs
- They are formed in lymph nodes, tonsils, appendix, spleen and other lymphatic organs.
- Lymphocytes are of 2 types. B & T lymphocytes also called B & T cells.
B lymphocytes
They originate in the embryo in the bone marrow. They then migrate and populate the lymph organs. They travel through blood stream to lymph nodes, tonsils, appendix, spleen, lymphatic nodules in intestine. As an adult three are no B lymphocytes in the bone marrow. They continue to multiply in the lymph organs.
B lymphocytes produce immunoglobulins or antibodies.
Action of Immunoglobulins or Antibodies
- Precipitation and Agglutination – Antibodies attach to foreign cells and cause them to clump. This is called agglutination. Antibodies can attach to bacteria and cause them to clump. They can attach to foreign RBCs and cause them to clump. This prevents them to go anywhere else in the body. It also makes it easy for a macrophage to eat it up.
- Antibodies can also attach to chemicals or toxins or viruses and cause them to clump together. This is called precipitation. It is similar to agglutination. The difference is that agglutination causes clumping of cells and precipitation causes clumping of something that is not a cell. - Opsonisation – Antibodies mark foreign agents for phagocytosis. They attract phagocytes to the foreign agents.
- Activate inflammatory response (by mast cells) & complement protein reaction
- Lysis – Antibodies can attach to bacterial cells and cause them to rupture. This is called lysis or cytolysis.
T Lymphocytes
These originate in the Thymus in the embryo.
Thymus is located in an embryo, foetus and a child between thyroid gland and the heart. It begins below the thyroid and extends all the way just above the heart in a child. The thymus degenerates at the beginning of puberty around the age of 12.
During childhood the thymus produces T lymphocytes which migrate to the lymphatic organs via the blood stream.
In lymph organs there are both B and T lymphocytes.
There are 2 main types of T lymphocytes.
Helper T cells. These are also called CD4 T cells or T-4 cells.
- These T cells release chemicals including interferon. Interferons are proteins which interfere with viral replication.
- These T cells release chemicals called cytokines.
- Cytokines activate B Lymphocytes and also cytotoxic T lymphocytes.
- When a B cell is activated its name changes to Plasma Cell.
Cytotoxic T Cells. Also called CD8 T Cells or T Killer Cells.
These release perforin proteins which causes rupture of foreign cells (cytolysis) and infected cells.
Lymphocytopenia – low lymphocyte count.
- One reason is chemotherapy.
- Another reason why only lymphocyte count is low but not other types of cells is HIV.
- HIV destroys helper T cells. Thus it reduces immunity and causes AIDS because now helper T cells cannot activate B cells to produce antibodies and T cells to cause cytolysis.
Lymphocytosis – Higher lymphocyte count.
- It is indicative of a viral infection.
- Higher Neutrophil count is indicative of a bacterial infection.
How does a Helper T cell get activated?
Macrophages swallow up a bacteria or a virus. The pieces of bacteria or virus appears on the surface of the macrophage. This is called an antigen epitope. It is basically a part of the chewed up virus or bacteria. These helper T cell makes contact with it and that activates it.