Red Flag = Serious Pathology
Why is it important to screen for Red Flags in Knee / Lower limb.
It is so because these red flags may require immediate referral.
- Fracture | Acute Trauma
- Infection (septic arthritis, osteomyelitis)
- Tumour
- Inflammatory Arthritis
- Deep Vein Thrombosis (DVT)
- Peripheral Vascular Disease
Fracture | Acute Trauma
Urgent referral is required for the following
- Suspected Fracture
- Suspected Quadriceps or Patellar tendon rupture
- First patellar dislocation
- Recurrent patellar dislocation with severe swelling
- Soft tissue injury with gross instability
- Neurovascular damage
- Suspected Slipped Capital Femoral Epiphyses
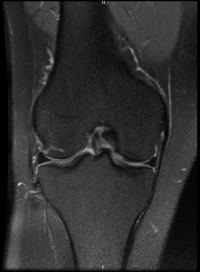
- Suspected osteonecrosis – SONK (spontaneous osteonecrosis of knee), also called subchondral insufficiency fracture
Infection
Urgent referral is required for suspected infection
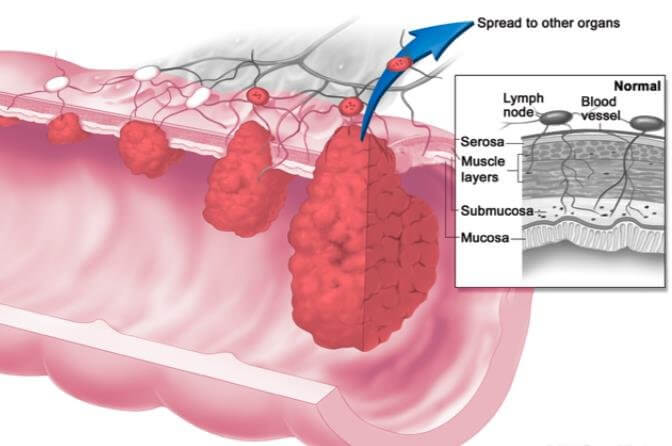
Tumour
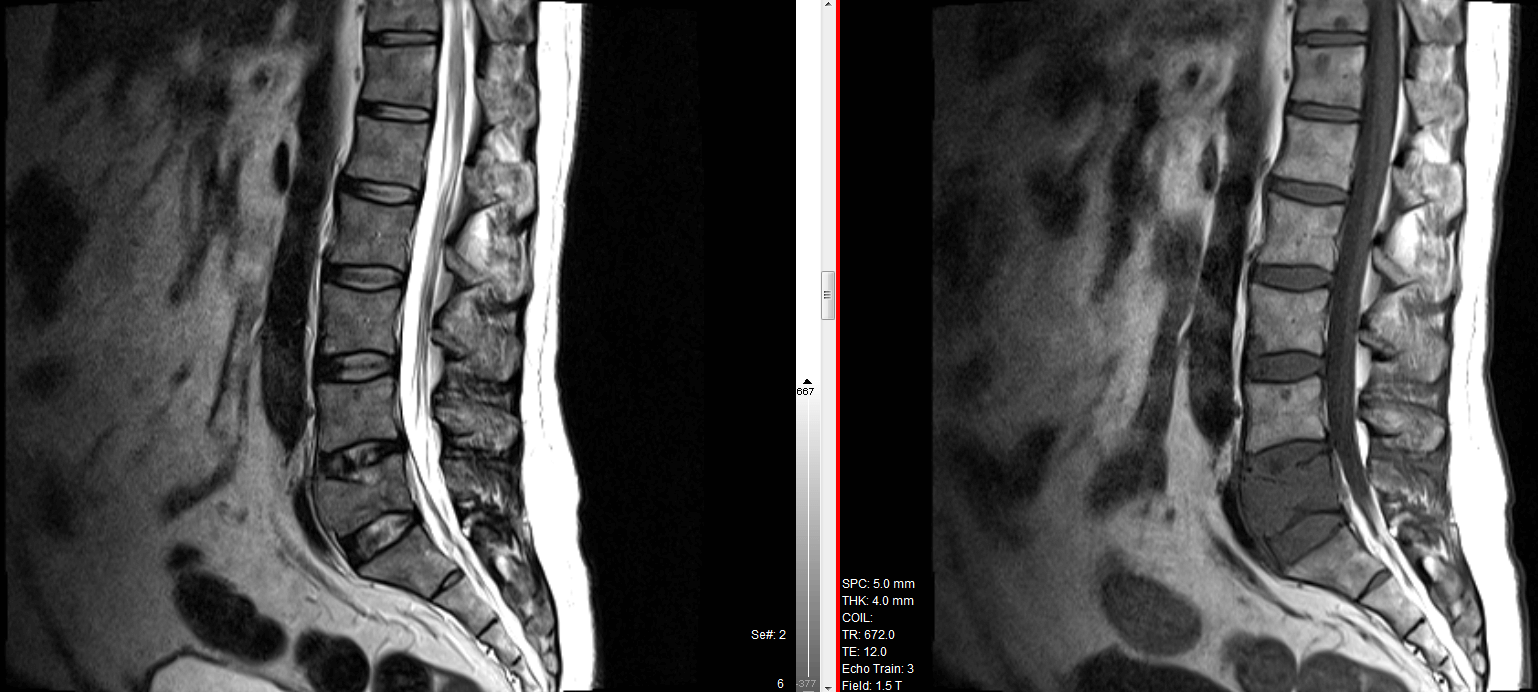
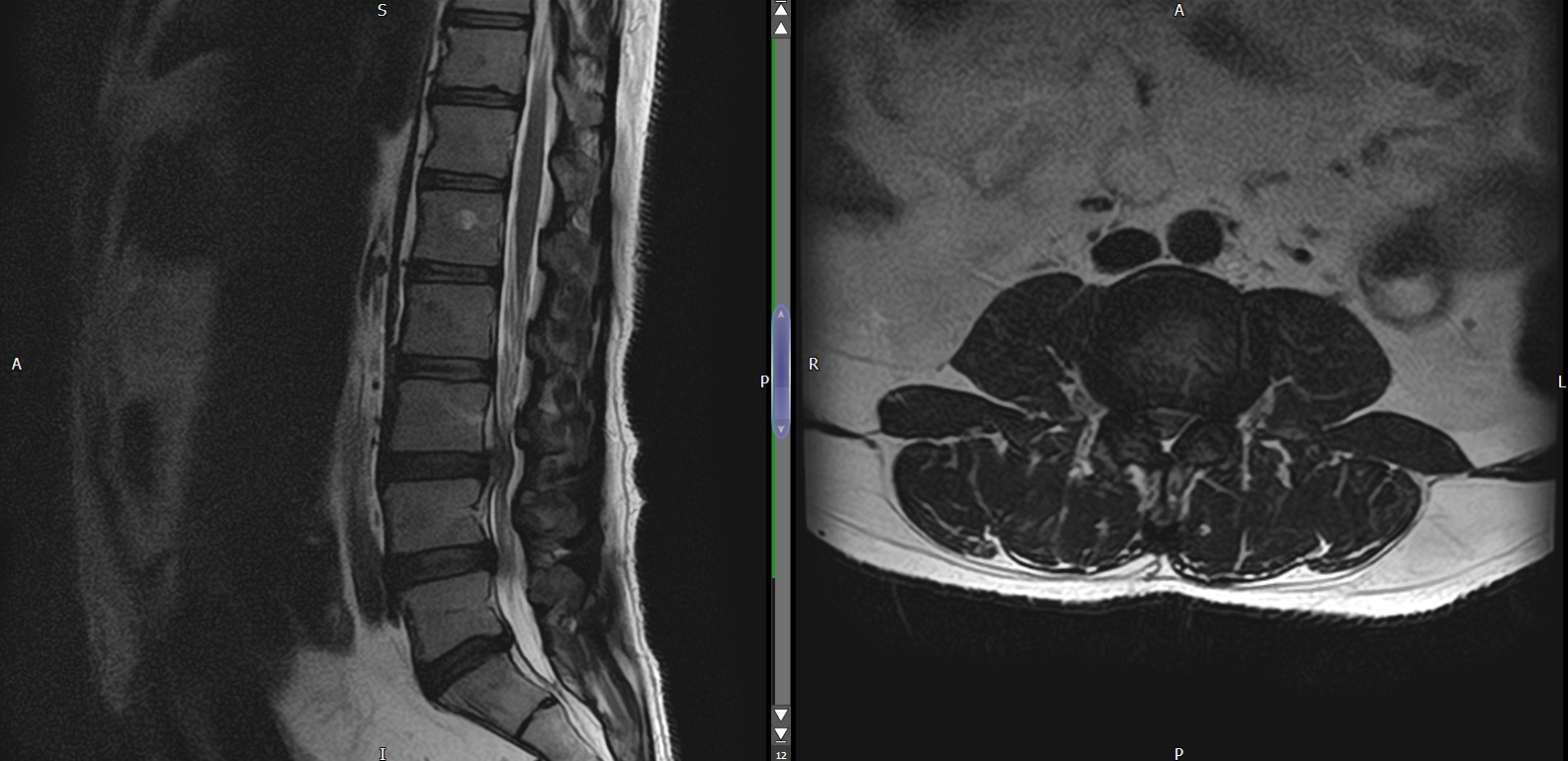
Urgent referral is required for suspected tumour. This could be
- Sarcoma (bone or soft tissue)
- Bone metastases
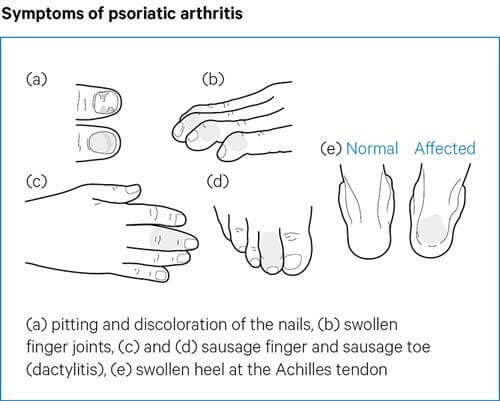
Inflammatory Arthritis / Polyarthritis
Urgent referral to rheumatology is required for suspected inflammatory polyarthritis.
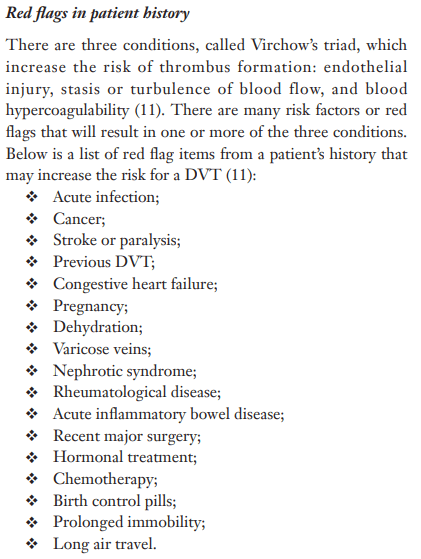
Deep Vein Thrombosis (DVT)
Timely detection of DVT can avoid Pulmonary Embolism (PE).
DVT Red flags in patient history
DVT Physical Exam
- Patient can be asymptomatic
- Symptomatic patients can have discoloration, pain, warmth, swelling, and tenderness of the affected extremity.
- Homan’s sign – pain and tenderness in the calf on passive dorsiflexion of the ankle with the knee extended. This test has poor diagnostic value.
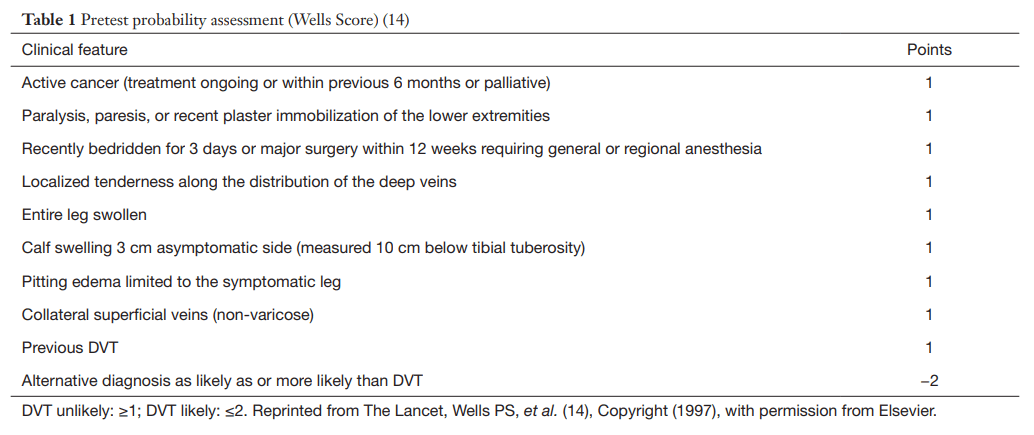
- Wells Score – validated for use in outpatient setting for suspicion of DVT.
Score < = 1 – DVT unlikely
Score > = 2 – DVT likely
Wells Score for Diagnosing Suspected DVT
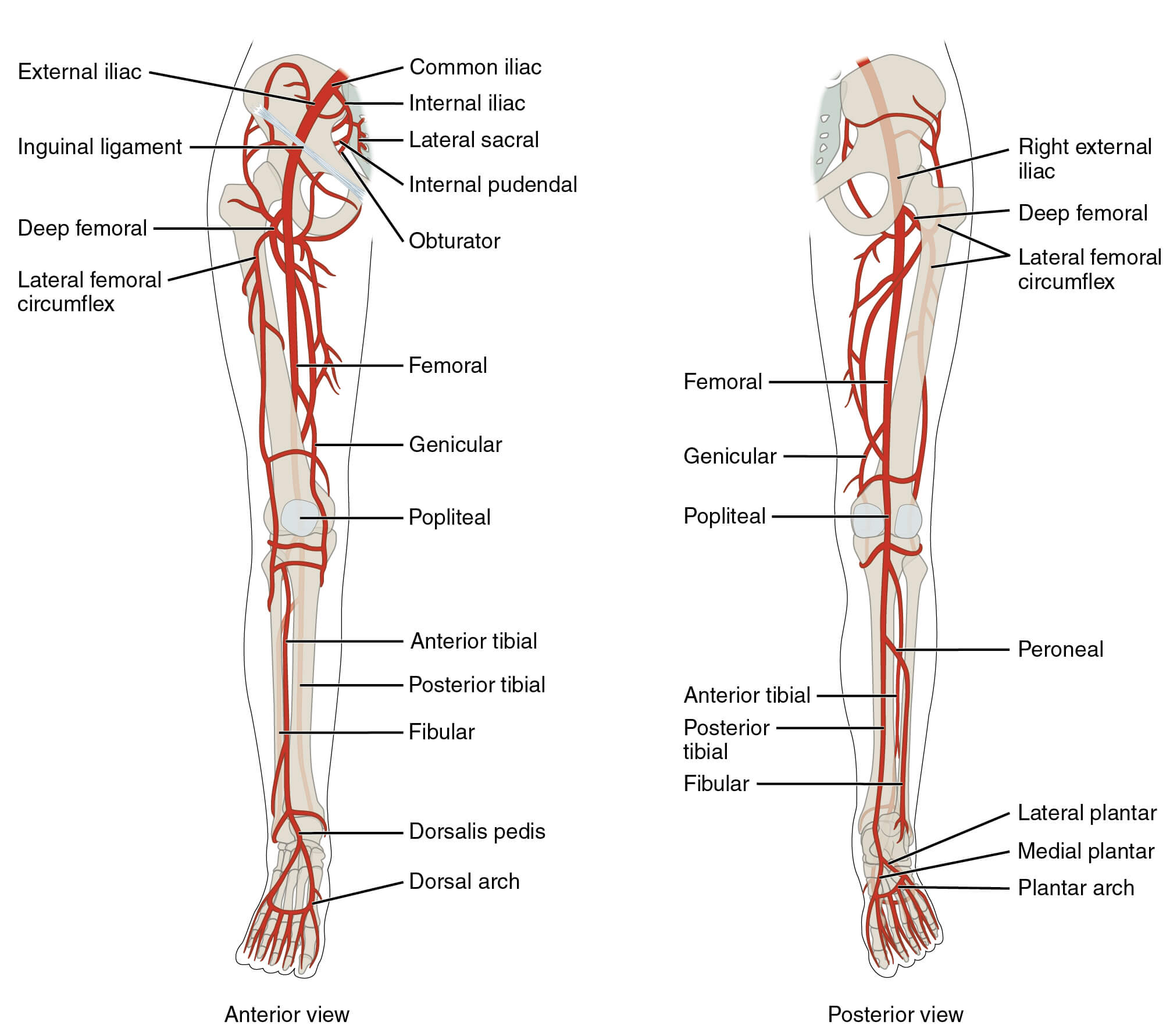
Peripheral Arterial Disease (PAD)
PAD = narrowing of arteries
Clinical feature – Intermittent claudication. This is pain and cramping in legs typically in calf muscles with exercise which eases with rest.
This is not an immediate emergency but timely recognition can avoid ischaemia related complications.
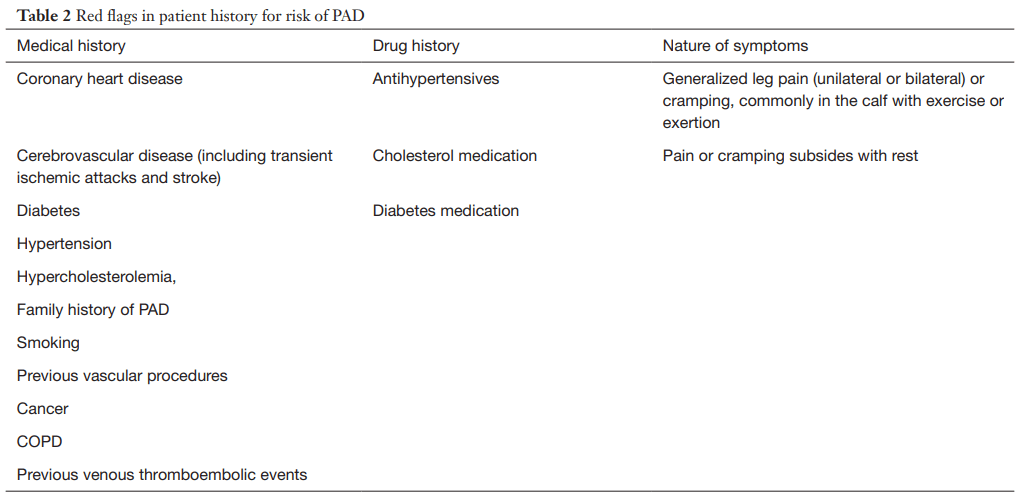
PAD Red Flags in Patient History
PAD Physical Exam
6 minute walk test
Ankle Brachial Index (ABI) –
Measurement of ABI = Highest ankle systolic blood pressure / Highest brachial systolic blood pressure. (measure BP at both arms and both ankles and take the highest reading for comparison)
- ABI values greater than 1.4 indicates calcification / vessel hardening. Refer to vascular specialist
- ABI Value 1 – 1.4 is considered normal.
- ABI Value 0.9 – 1 is acceptable/borderline.
- ABI Value 0.8 - 0.9 suggests some arterial disease. Treat risk factors.
- ABI Value 0.4 - 0.8 suggests moderate arterial disease. Refer to vascular specialist.
- ABI Value less than 0.4 suggests severe arterial disease. Refer to vascular specialist.
PAD Assessment
Read more:
- Non Invasive Physiologic Vascular Studies: A guide to diagnosing peripheral arterial disease
- Identifying peripheral arterial diseases or flow limitations of the lower limb 2022
- The Role of Ankle-Brachial Index for Predicting Peripheral Arterial Disease 2014